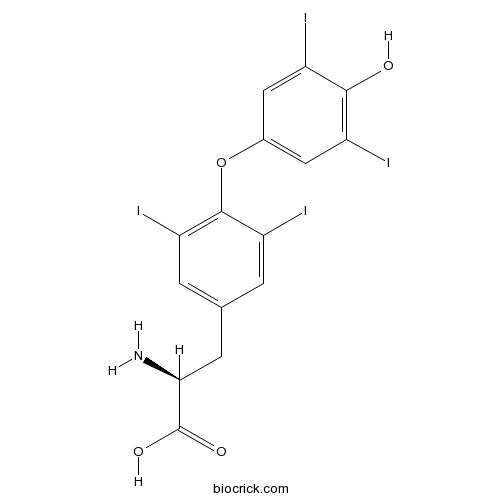
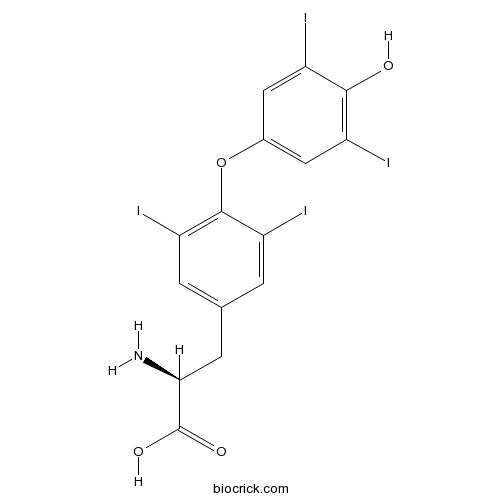
L-ThyroxineIodine containing hormone CAS# 51-48-9 |
- Dexpramipexole dihydrochloride
Catalog No.:BCC1528
CAS No.:104632-27-1
- Dexpramipexole
Catalog No.:BCC1527
CAS No.:104632-28-2
- Cariprazine hydrochloride
Catalog No.:BCC1454
CAS No.:1083076-69-0
- Cariprazine
Catalog No.:BCC1453
CAS No.:839712-12-8
Quality Control & MSDS
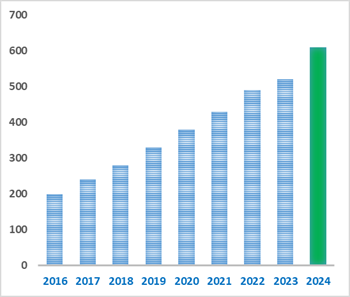
Number of papers citing our products
Chemical structure
3D structure
| Cas No. | 51-48-9 | SDF | Download SDF |
| PubChem ID | 5819 | Appearance | Powder |
| Formula | C15H11I4NO4 | M.Wt | 776.87 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Synonyms | Levothyroxine; T4 | ||
| Solubility | DMSO : ≥ 28 mg/mL (36.04 mM) *"≥" means soluble, but saturation unknown. | ||
| Chemical Name | (2S)-2-amino-3-[4-(4-hydroxy-3,5-diiodophenoxy)-3,5-diiodophenyl]propanoic acid | ||
| SMILES | NC(Cc1cc(I)c(Oc2cc(I)c(O)c(I)c2)c(I)c1)C(O)=O | ||
| Standard InChIKey | XUIIKFGFIJCVMT-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C15H11I4NO4/c16-8-4-7(5-9(17)13(8)21)24-14-10(18)1-6(2-11(14)19)3-12(20)15(22)23/h1-2,4-5,12,21H,3,20H2,(H,22,23) | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | L-Thyroxine (Levothyroxine; T4) is a synthetic hormone in the treatment of hypothyroidism. DIO enzymes convert biologically active thyroid hormone (Triiodothyronine,T3) from L-Thyroxine (T4).In Vivo:Deiodinases (DIOs), which catalyse the conversion of thyroxine (pro-hormone) to the active thyroid hormone, are associated with thyroid stimulating hormone (TSH) levels. DIO1 and DIO2 catalyze activation of thyroid hormone secretion in contrast to DIO3 playing role inactivation of the secretion. Activities of DIO1 and DIO2 play pivotal role in the negative feedback regulation of pituitary TSH secretion[1]. L-Thyroxine (T4) and Triiodothyronine (T3) hormones are known to modulate the expression of ionic channels, pumps and regulatory contractile proteins. Moreover, thyroid hormones have been shown to influence calcium homeostasis and flux responsible for excitation and contractility, with L-Thyroxine and Triiodothyronine modulating its pharmacological control and secretion. In rats fed 12 weeks with the iodine-free diet, a significant decrease in the levels of both Triiodothyronine and L-Thyroxine is observed when compared to the control group fed with standard diet (p<0.001). In the group treated with low doses of L-Thyroxine, an increase in L-Thyroxine levels is observed (p=0.02) while Triiodothyronine levels remain virtually similar to the control group (p=0.19). Rats treated with high doses of L-Thyroxine display a significant increase in both Triiodothyronine and L-Thyroxine circulating concentrations compared to the non-treated hypothyroid group (p<0.001 and p=0.004, respectively) and a significant increase in L-Thyroxine levels when compared to the control values (p=0.03)[2]. References: | |||||

L-Thyroxine Dilution Calculator

L-Thyroxine Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 1.2872 mL | 6.4361 mL | 12.8722 mL | 25.7443 mL | 32.1804 mL |
| 5 mM | 0.2574 mL | 1.2872 mL | 2.5744 mL | 5.1489 mL | 6.4361 mL |
| 10 mM | 0.1287 mL | 0.6436 mL | 1.2872 mL | 2.5744 mL | 3.218 mL |
| 50 mM | 0.0257 mL | 0.1287 mL | 0.2574 mL | 0.5149 mL | 0.6436 mL |
| 100 mM | 0.0129 mL | 0.0644 mL | 0.1287 mL | 0.2574 mL | 0.3218 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||
Calcutta University

University of Minnesota

University of Maryland School of Medicine
University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University
DRURY University
Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University
The University of Tokyo

Korea University
L-Thyroxine is an iodine containing hormone produced from thyroglobulin in the thyroid follicular cells. L-Thyroxine reduces total cholesterol level, low-density lipoprotein cholesterol as well as waist to hip ratio in subclinical hypothyroidism pateints.
- Histamine
Catalog No.:BCN2188
CAS No.:51-45-6
- Adrenaline
Catalog No.:BCN2191
CAS No.:51-43-4
- Epinephrine Bitartrate
Catalog No.:BCC4348
CAS No.:51-42-3
- Norepinephrine
Catalog No.:BCN2206
CAS No.:51-41-2
- H-Hyp-OH
Catalog No.:BCC3250
CAS No.:51-35-4
- Scopolamine
Catalog No.:BCN5045
CAS No.:51-34-3
- Isoprenaline HCl
Catalog No.:BCC4328
CAS No.:51-30-9
- Tiratricol
Catalog No.:BCC4738
CAS No.:51-24-1
- Fluorouracil (Adrucil)
Catalog No.:BCC2135
CAS No.:51-21-8
- Benzimidazole
Catalog No.:BCC8847
CAS No.:51-17-2
- Procaine HCl
Catalog No.:BCC5072
CAS No.:51-05-8
- Pronethalol hydrochloride
Catalog No.:BCC5678
CAS No.:51-02-5
- Propylthiouracil
Catalog No.:BCC4931
CAS No.:51-52-5
- Atropine
Catalog No.:BCN5639
CAS No.:51-55-8
- Homatropine Bromide
Catalog No.:BCC4570
CAS No.:51-56-9
- D-Amphetamine sulfate
Catalog No.:BCC5942
CAS No.:51-63-8
- 4'-Methoxyacetanilide
Catalog No.:BCC8711
CAS No.:51-66-1
- Tyramine
Catalog No.:BCN6776
CAS No.:51-67-2
- Carbamoylcholine chloride
Catalog No.:BCC7492
CAS No.:51-83-2
- (2-Acetoxyethyl)trimethylammonium
Catalog No.:BCN1743
CAS No.:51-84-3
- Tetramethylammonium
Catalog No.:BCN1816
CAS No.:51-92-3
- Trachelanthine
Catalog No.:BCN2042
CAS No.:510-19-0
- Voacangine
Catalog No.:BCN3224
CAS No.:510-22-5
- Belladonnine
Catalog No.:BCN1892
CAS No.:510-25-8
The effect of l-thyroxine treatment on sexual function and depressive symptoms in men with autoimmune hypothyroidism.[Pubmed:28315587]
Pharmacol Rep. 2017 Jun;69(3):432-437.
BACKGROUND: Thyroid autoimmunity and mild hypothyroidism in women seem to be associated with sexual dysfunction and depressive symptoms. Data concerning similar associations in men are limited. The aim of this study was to investigate sexual functioning and depressive symptoms in men with autoimmune hypothyroidism. METHODS: The study population consisted of three groups: men with autoimmune overt hypothyroidism (group A), men with autoimmune subclinical hypothyroidism (group B) and healthy euthyroid males without thyroid autoimmunity (group C). Apart from measuring serum levels of thyrotropin and free thyroid hormones and thyroid antibody titers, all included patients completed a questionnaires evaluating male sexual function (International Index of Erectile Function-15: IIEF-15) and assessing the presence and severity of depressive symptoms (Beck Depression Inventory-Second Edition - BDI-II) before and after 6 months of levothyroxine treatment. RESULTS: Men with overt hypothyroidism obtained lower scores in all five domains of IIEF-15, while men with subclinical hypothyroidism only in erectile function. The total BDI-II score was higher in groups A than in groups B and C, as well as higher in group B than in group C. L-Thyroxine improved erectile function and normalized intercourse satisfaction, orgasmic function, sexual desire and overall satisfaction in group A, as well as normalized erectile function in group B. In group A, L-Thyroxine reduced, while in group B tended to reduce total BDI-II. CONCLUSIONS: The obtained results suggest that autoimmune hypothyroidism in men is characterized by sexual and mood disturbances and that hypothyroid patients with sexual dysfunction and depressive symptoms benefit from L-Thyroxine treatment.
Thyroid function in children and adolescents with Hashimoto's thyroiditis after l-thyroxine discontinuation.[Pubmed:28348002]
Endocr Connect. 2017 May;6(4):206-212.
OBJECTIVE: Thyroid function may recover in patients with Hashimoto's thyroiditis (HT). DESIGN: To investigate thyroid function and the need to resume L-Thyroxine treatment after its discontinuation. SETTING: Nine Italian pediatric endocrinology centers. PATIENTS: 148 children and adolescents (25 m and 123 f) with HT on treatment with L-Thyroxine for at least one year. INTERVENTION AND MAIN OUTCOME MEASURE: Treatment was discontinued in all patients, and serum TSH and fT4 concentrations were measured at the time of treatment discontinuation and then after 2, 6, 12 and 24 months. Therapy with L-Thyroxine was re-instituted when TSH rose >10 U/L and/or fT4 was below the normal range. The patients were followed up when TSH concentrations were between 5 and 10 U/L and fT4 was in the normal range. RESULTS: At baseline, TSH was in the normal range in 139 patients, and was between 5 and 10 U/L in 9 patients. Treatment was re-instituted after 2 months in 37 (25.5%) patients, after 6 months in 13 patients (6.99%), after 12 months in 12 patients (8.6%), and after 24 months in an additional 3 patients (3.1%). At 24 months, 34 patients (34.3%) still required no treatment. TSH concentration >10 U/L at the time of diagnosis was the only predictive factor for the deterioration of thyroid function after L-Thyroxine discontinuation. CONCLUSIONS: This study confirms that not all children with HT need life-long therapy with L-Thyroxine, and the discontinuation of treatment in patients with a TSH level <10 U/L at the time of diagnosis should be considered.
Effects of L-thyroxine treatment on heart functions in infants with congenital hypothyroidism.[Pubmed:28358714]
J Pediatr Endocrinol Metab. 2017 May 1;30(5):557-560.
BACKGROUND: Impaired heart functions in newborns with hypothyroidism should be reversed by levothyroxine substitution therapy. The aim of the study was to investigate heart functions with congenital hypothroidism (CH) in newborns and changes after levothyroxine substitution therapy, measured with tissue Doppler echocardiography and conventional echocardiography. METHODS: The study included 30 neonates with CH and 34 healthy controls. Echocardiography were performed at baseline, 2nd week and 6th month of therapy. RESULTS: Heart systolic function was normal. Mitral E velocities and mitral E/A ratios were significantly lower in patients at baseline. Tei indices were significantly higher in patients and a significant negative correlation was detected between free thyroxine levels and Tei indices.When early and late post-treatment echocardiography findings are compared, a non-significant difference was detected. CONCLUSIONS: Neonates with CH may exhibit systolic and diastolic heart dysfunction, which can be reversed by early L-T4 substitution treatment. The Tei index index should be measured in addition to conventional echocardiography.
Alteration of Hemostatic Parameters in Patients with Different Levels of Subclinical Hypothyroidism and the Effect of L-thyroxine Treatment.[Pubmed:28249913]
Ann Clin Lab Sci. 2017 Jan;47(1):29-35.
Subclinical hypothyroidism (SH) is associated with hypercoagulability and hypofibrinolysis. The objective of this study was to assess the effect of L-Thyroxine (L-T4) treatment and to evaluate changes in the hemostatic abnormalities of patients with varying severities of SH. We measured tissue plasminogen activator (t-PA), plasminogen activator inhibitor-1 (PAI-1), D-dimer (DDI), fibrinogen (FIB), platelet counts (PLT), mean platelet volume (MPV), platelet distribution width (PDW), activated partial thromboplastin time (APTT), and prothrombin time (PT) in 149 female subjects. The prospective study included 54 patients in the control group, 53 patients with 4.2 muIU/mL


