CHCMCT inhibitor; decreases glycoloysis CAS# 28166-41-8 |
- Resminostat hydrochloride
Catalog No.:BCC1888
CAS No.:1187075-34-8
- RG2833
Catalog No.:BCC1893
CAS No.:1215493-56-3
- Rocilinostat (ACY-1215)
Catalog No.:BCC2144
CAS No.:1316214-52-4
- Daminozide
Catalog No.:BCC1514
CAS No.:1596-84-5
- Tasquinimod
Catalog No.:BCC1987
CAS No.:254964-60-8
Quality Control & MSDS
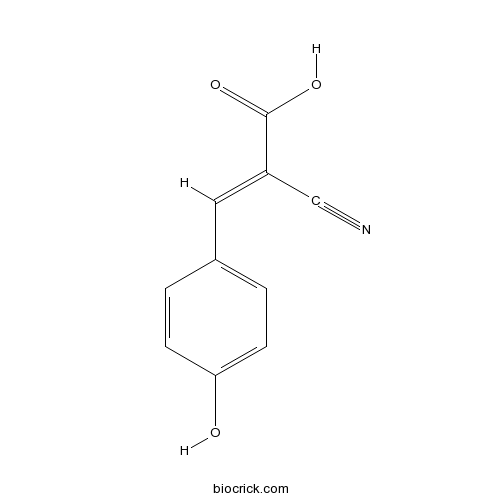
3D structure
Package In Stock
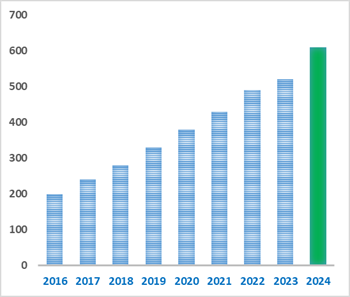
Number of papers citing our products
| Cas No. | 28166-41-8 | SDF | Download SDF |
| PubChem ID | 5328791 | Appearance | Powder |
| Formula | C10H7NO3 | M.Wt | 189.17 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | Soluble to 100 mM in DMSO and to 50 mM in ethanol | ||
| Chemical Name | (E)-2-cyano-3-(4-hydroxyphenyl)prop-2-enoic acid | ||
| SMILES | C1=CC(=CC=C1C=C(C#N)C(=O)O)O | ||
| Standard InChIKey | AFVLVVWMAFSXCK-VMPITWQZSA-N | ||
| Standard InChI | InChI=1S/C10H7NO3/c11-6-8(10(13)14)5-7-1-3-9(12)4-2-7/h1-5,12H,(H,13,14)/b8-5+ | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Monocarboxylic acid transport (MCT) inhibitor. Exhibits antitumoral and antiangiogenic activity in gliomas in vivo; decreases glycolytic metabolism, migration, and invasion in U251 cells. Enhances the effect of antitumor agent temozolomide. Blocks lactate efflux from glioma cells and sensitizes cells to irradiation. |

CHC Dilution Calculator

CHC Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 5.2863 mL | 26.4313 mL | 52.8625 mL | 105.725 mL | 132.1563 mL |
| 5 mM | 1.0573 mL | 5.2863 mL | 10.5725 mL | 21.145 mL | 26.4313 mL |
| 10 mM | 0.5286 mL | 2.6431 mL | 5.2863 mL | 10.5725 mL | 13.2156 mL |
| 50 mM | 0.1057 mL | 0.5286 mL | 1.0573 mL | 2.1145 mL | 2.6431 mL |
| 100 mM | 0.0529 mL | 0.2643 mL | 0.5286 mL | 1.0573 mL | 1.3216 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||
Calcutta University

University of Minnesota

University of Maryland School of Medicine
University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University
DRURY University
Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University
The University of Tokyo

Korea University
- Peonidin-3-O-galactoside chloride
Catalog No.:BCN3027
CAS No.:28148-89-2
- 8-Aminoadenine
Catalog No.:BCC6108
CAS No.:28128-33-8
- H-Pro-OtBu
Catalog No.:BCC3020
CAS No.:2812-46-6
- Pluviatolide
Catalog No.:BCN3041
CAS No.:28115-68-6
- Adamantane
Catalog No.:BCN8481
CAS No.:281-23-2
- Chaetocin
Catalog No.:BCC2429
CAS No.:28097-03-2
- (+)-Ulopterol
Catalog No.:BCN1228
CAS No.:28095-18-3
- A 286982
Catalog No.:BCC3946
CAS No.:280749-17-9
- SB 216763
Catalog No.:BCC3650
CAS No.:280744-09-4
- VUF 5574
Catalog No.:BCC7030
CAS No.:280570-45-8
- Rediocide A
Catalog No.:BCN5175
CAS No.:280565-85-7
- Piperazine Ferulate
Catalog No.:BCN3277
CAS No.:171876-65-6
- Futoquinol
Catalog No.:BCN6416
CAS No.:28178-92-9
- 5-Amino-2-mercaptobenzimidazole
Catalog No.:BCC8730
CAS No.:2818-66-8
- Sinensin
Catalog No.:BCN4797
CAS No.:28189-90-4
- Dihydrodehydrodiconiferyl alcohol
Catalog No.:BCN5176
CAS No.:28199-69-1
- Lauterine
Catalog No.:BCN7062
CAS No.:28200-65-9
- JTE 907
Catalog No.:BCC7380
CAS No.:282089-49-0
- Phlorin
Catalog No.:BCN5177
CAS No.:28217-60-9
- HOOBt
Catalog No.:BCC2817
CAS No.:28230-32-2
- Reynosin
Catalog No.:BCN5178
CAS No.:28254-53-7
- Tyrphostin A1
Catalog No.:BCC5404
CAS No.:2826-26-8
- Baicalein 6-O-glucoside
Catalog No.:BCN3325
CAS No.:28279-72-3
- Beta-Elemonic acid
Catalog No.:BCN2981
CAS No.:28282-25-9
Viability of pegIFNalpha-RBV for CHC in the direct acting antiviral era: a practical algorithm between efficacy and cost containment.[Pubmed:27351356]
J Chemother. 2017 Apr;29(2):94-101.
The classical pegylated interferon alpha (peg-IFNalpha) and ribavirin (RBV) treatment of chronic hepatitis C (CHC) is progressively being replaced by new direct acting antivirals, whose costs remain a major barrier to widespread use. Using baseline data and viral kinetics, we developed a predictive algorithm to allocate to DAA patients who are not going to respond to peg-IFNalpha/RBV. This prospective study evaluated 205 CHC patients treated with peg-IFNalpha/RBV. HCVRNA kinetics during the initial 3 days of therapy and baseline variables including age, genotype, fibrosis and ALTs were used to construct a prediction rule in terms of sustained virological response (SVR). One hundred and twenty-one patients achieved an SVR (59%). Variables independently associated with SVR were HCVRNA, ALT, glycaemia, viral genotype, and fibrosis. The decline of viremia from baseline to 48/72 h was significantly different in SVR compared to non-SVR patients (2.2 vs. 0.65 log10 IU/mL; p < 0.001), and was influenced by viral genotype, levels of ALT, stage of fibrosis and IL28B polymorphism. In genotype 1, HCVRNA decline <0.8 logs had a negative predictive value of 90%, and in genotype 2, HCVRNA decline >1.2 logs had a positive predictive value of 92%. A combination of HCVRNA kinetics and a score based on pre-treatment parameters was highly accurate in predicting SVR in most patients. Outcome of peg-IFNalpha/RBV treatment may be predicted combining evaluation of baseline variables and HCVRNA kinetics. This allows to individualize treatment, reserving newer and more expensive DAAs to CHC patients who are in most need of them.
Long-term outcome of chronic hepatitis C virus infection in a real-world setting: The German LOTOS study.[Pubmed:28247572]
Liver Int. 2017 Oct;37(10):1468-1475.
BACKGROUND & AIMS: There are few large-scale, prospective studies comparing liver-associated events in treated and untreated patients with CHC managed in routine clinical practice. METHODS: Patients with CHC were prospectively enrolled in a non-interventional study. Data from patients with available documentation who had either achieved a sustained virological response, or were non-responders, relapsers, or had virological breakthrough following treatment with peginterferon alfa-2a+/-ribavirin, or who had been diagnosed but never treated at least 3 years previously, and who remained under medical observation were analyzed. Primary endpoint was liver-associated events (composite of decompensation/liver failure, ascites, hepatocellular carcinoma, or liver transplant/placement on a transplant list). RESULTS: In all, 1444 eligible patients were identified. Mean follow-up was 4.7 (standard deviation; SD 1.1) years. Patients with sustained virological response had a lower incidence of liver-associated events vs non-responders, relapsers, or virological breakthrough and never treated patients (1.7% vs 4.7% and 4.7% respectively). The proportion of patients with cirrhosis increased from baseline in the non-responders, relapsers, or virological breakthrough (6.8%-10.5%) and never treated group (3.7%-8.4%), with an associated increase in severity, but was unchanged in the sustained virological response group (2.1%). Event-free survival was significantly higher in sustained virological response patients (P=.0082). CONCLUSIONS: In this "real-world" cohort, the achievement of sustained virological response almost eliminated liver-related morbidity and mortality compared with patients who failed to achieve sustained virological response and those who were untreated. Overall, the LOTOS cohort highlights the importance of timely and effective treatment for patients with CHC.
Combined hormonal contraceptive (CHC) use among obese women and contraceptive effectiveness: a systematic review.[Pubmed:27823942]
Contraception. 2017 Feb;95(2):117-129.
OBJECTIVE: To evaluate from the literature whether combined hormonal contraception (CHC), including combined oral contraception pills (COCs), transdermal patch, vaginal ring or combined injectables, have different effectiveness or failure rates by body weight or body mass index (BMI). STUDY DESIGN: We searched PubMed and the Cochrane Library databases for all articles in all languages published between inception and February 2016, for evidence relevant to body weight or BMI, CHC use and contraceptive effectiveness. The quality of each individual study was assessed using the system for evaluating evidence developed by the United States Preventive Services Task Force. RESULTS: From 2874 articles, we identified 15 reports for inclusion, all of fair to poor quality. Fourteen studies measured the association of obesity status and contraceptive failure among COC users. Three fair quality and one poor quality study reported increased COC failure among a heterogeneous population of overweight and obese women compared with normal weight women, while eight fair quality and two poor quality studies did not find an association. Two fair quality studies reported on contraceptive transdermal patches. One pooled analysis described a higher proportion of pregnancies among women using the patch who weighed >/=90 kg; another secondary analysis suggested BMI>30 was associated with increased failure. No studies directly compared contraceptive effectiveness using the combined vaginal ring or combined injectable. CONCLUSION: Current available evidence addressing the risk of CHC failure in obese compared to normal weight women is limited to fair and poor quality studies. Studies of COCs show mixed results, though absolute differences in COC failure by body weight and BMI are small. Based on limited evidence, it appears that increasing body weight and BMI may contribute to decreasing contraceptive patch effectiveness.
MONOCYTE CHEMOTACTIC PROTEIN AND RESPONSE TO PEGYLATED INTERFERON-ALPHA-2A TREATMENT IN PATIENTS WITH CHRONIC HEPATITIS C (CHC) GENOTYPE 4.[Pubmed:27363047]
J Egypt Soc Parasitol. 2016 Apr;46(1):117-24.
The prevalence of hepatitis C virus (HCV) infection varies across the world, with the highest number of infections reported in Egypt. Monocyte chemotactic protein-1 (MCP-1) is a potent chemokine, and its hepatic expression is up-regulated during chronic HCV infection. Fifty naive patients with chronic hepatitis C in National Hepatology & Tropical Medicine Research Institute and 20 healthy volunteers as controls were enrolled in a prospective study designed with strict inclusion criteria to nullify the effect of confounding variables and further minimize selection bias. Fifty naive patients were treated with PEG-IFN-a2b, at a dose of 1801 g/kg subcutaneously every week plus ribavirin at a dose of 1000- 1200 mg/day, according to the patient's body weight, for 48 weeks. Quantification of HCV-RNA by real-time PCR and MCP-1 by ELISA were performed for every patient and controls. There was a sta- tistically significant difference between patients and control group as regards the quantity of MCP-1 (P < 0.05) (Mann-Whitney test) (P = 0.004). There was a significant difference between responders and nonresponses regarding MCP-1 (P < 0.05), responders showed a higher percentage of cases with initial MCP-1 < 306 (P < 0.05). We conclude the importance of the detection of MCP-1 expression at the start of therapy as a factor for assessing the likelihood of HCV genotype 4 patients to achieving a sustained virological response to treatment with IFN-a2 in combination with ribavirin.
Monocarboxylate transporters (MCTs) in gliomas: expression and exploitation as therapeutic targets.[Pubmed:23258846]
Neuro Oncol. 2013 Feb;15(2):172-88.
BACKGROUND: Gliomas exhibit high glycolytic rates, and monocarboxylate transporters (MCTs) play a major role in the maintenance of the glycolytic metabolism through the proton-linked transmembrane transport of lactate. However, their role in gliomas is poorly studied. Thus, we aimed to characterize the expression of MCT1, MCT4, and their chaperone CD147 and to assess the therapeutic impact of MCT inhibition in gliomas. METHODS: MCTs and CD147 expressions were characterized by immunohistochemistry in nonneoplastic brain and glioma samples. The effect of CHC (MCT inhibitor) and MCT1 silencing was assessed in in vitro and in vivo glioblastoma models. RESULTS: MCT1, MCT4, and CD147 were overexpressed in the plasma membrane of glioblastomas, compared with diffuse astrocytomas and nonneoplastic brain. CHC decreased glycolytic metabolism, migration, and invasion and induced cell death in U251 cells (more glycolytic) but only affected proliferation in SW1088 (more oxidative). The effectiveness of CHC in glioma cells appears to be dependent on MCT membrane expression. MCT1 downregulation showed similar effects on different glioma cells, supporting CHC as an MCT1 inhibitor. There was a synergistic effect when combining CHC with temozolomide treatment in U251 cells. In the CAM in vivo model, CHC decreased the size of tumors and the number of blood vessels formed. CONCLUSIONS: This is the most comprehensive study reporting the expression of MCTs and CD147 in gliomas. The MCT1 inhibitor CHC exhibited anti-tumoral and anti-angiogenic activity in gliomas and, of importance, enhanced the effect of temozolomide. Thus, our results suggest that development of therapeutic approaches targeting MCT1 may be a promising strategy in glioblastoma treatment.
Metabolic remodeling of malignant gliomas for enhanced sensitization during radiotherapy: an in vitro study.[Pubmed:17277695]
Neurosurgery. 2006 Dec;59(6):1313-23; discussion 1323-4.
OBJECTIVE: To investigate a novel method to enhance radiosensitivity of gliomas via modification of metabolite flux immediately before radiotherapy. Malignant gliomas are highly glycolytic and produce copious amounts of lactic acid, which is effluxed to the tumor microenvironment via lactate transporters. We hypothesized that inhibition of lactic acid efflux would alter glioma metabolite profiles, including those that are radioprotective. H magnetic resonance spectroscopy (MRS) was used to quantify key metabolites, including those most effective for induction of low-dose radiation-induced cell death. METHODS: We inhibited lactate transport in U87-MG gliomas with alpha-cyano-4-hydroxycinnamic acid (ACCA). Flow cytometry was used to assess induction of cell death in treated cells. Cells were analyzed by MRS after ACCA treatment. Control and treated cells were subjected to low-dose irradiation, and the surviving fractions of cells were determined by clonogenic assays. RESULTS: MRS revealed changes to intracellular lactate on treatment with ACCA. Significant decreases in the metabolites taurine, glutamate, glutathione, alanine, and glycine were observed, along with inversion of the choline/phosphocholine profile. On exposure to low-dose radiation, ACCA-pretreated U-87MG cells underwent rapid morphological changes, which were followed by apoptotic cell death. CONCLUSION: Inhibition of lactate efflux in malignant gliomas results in alterations of glycolytic metabolism, including decreased levels of the antioxidants taurine and glutathione and enhanced radiosensitivity of ACCA-treated cells. Thus, in situ application of lactate transport inhibitors such as ACCA as a novel adjunctive therapeutic strategy against glial tumors may greatly enhance the level of radiation-induced cell killing during a combined radio- and chemotherapeutic regimen.
The H+-linked monocarboxylate transporter (MCT1/SLC16A1): a potential therapeutic target for high-risk neuroblastoma.[Pubmed:17000864]
Mol Pharmacol. 2006 Dec;70(6):2108-15.
Neuroblastomas produce high amounts of lactic acid and upregulate the H(+)-linked monocarboxylate transporter isoform 1 (MCT1/SLC16A1). We found elevated MCT1 mRNA levels in fresh neuroblastoma biopsy samples that correlated positively with risk of fatal disease and amplification of the "proto-oncogenic" transcription factor MYCN. We further investigated MCT as a potential therapeutic target in vitro. The neuroblastoma cell lines evaluated were Sk-N-SH, CHP134, IMR32, and NGP. All lines exhibited decreased intracellular pH at low tumor-like extracellular pH. Lonidamine or exogenous lactate further lowered intracellular pH. Immediate early lowering of intracellular pH with lonidamine or lactate at extracellular pH 6.5 correlated positively with diminished cell viability within 48 h. These findings indicate that MCT1 is a potential therapeutic target and that neuroblastoma therapy may be enhanced by therapeutic strategies to inhibit or overwhelm MCT. Additional experiments indicated that the mechanism of cell death by lonidamine or exogenous lactate is similar to that obtained using alpha-cyano-4-OH-cinnamate, a well established MCT inhibitor. Because lactate production is also high in melanoma and many other tumor types, MCT inhibitors may have broad application in cancer treatment. Such treatment would have selectivity by virtue of the acidic milieu surrounding tumors, because MCT is increasingly active as extracellular pH decreases below 7.0 and lactic acid production increases.
The low-affinity monocarboxylate transporter MCT4 is adapted to the export of lactate in highly glycolytic cells.[Pubmed:10926847]
Biochem J. 2000 Aug 15;350 Pt 1:219-27.
Transport of lactate and other monocarboxylates in mammalian cells is mediated by a family of transporters, designated monocarboxylate transporters (MCTs). The MCT4 member of this family has recently been identified as the major isoform of white muscle cells, mediating lactate efflux out of glycolytically active myocytes [Wilson, Jackson, Heddle, Price, Pilegaard, Juel, Bonen, Montgomery, Hutter and Halestrap (1998) J. Biol. Chem. 273, 15920-15926]. To analyse the functional properties of this transporter, rat MCT4 was expressed in Xenopus laevis oocytes and transport activity was monitored by flux measurements with radioactive tracers and by changes of the cytosolic pH using pH-sensitive microelectrodes. Similar to other members of this family, monocarboxylate transport via MCT4 is accompanied by the transport of H(+) across the plasma membrane. Uptake of lactate strongly increased with decreasing extracellular pH, which resulted from a concomitant drop in the K(m) value. MCT4 could be distinguished from the other isoforms mainly in two respects. First, MCT4 is a low-affinity MCT: for L-lactate K(m) values of 17+/-3 mM (pH-electrode) and 34+/-5 mM (flux measurements with L-[U-(14)C]lactate) were determined. Secondly, lactate is the preferred substrate of MCT4. K(m) values of other monocarboxylates were either similar to the K(m) value for lactate (pyruvate, 2-oxoisohexanoate, 2-oxoisopentanoate, acetoacetate) or displayed much lower affinity for the transporter (beta-hydroxybutyrate and short-chain fatty acids). Under physiological conditions, rat MCT will therefore preferentially transport lactate. Monocarboxylate transport via MCT4 could be competitively inhibited by alpha-cyano-4-hydroxycinnamate, phloretin and partly by 4, 4'-di-isothiocyanostilbene-2,2'-disulphonic acid. Similar to MCT1, monocarboxylate transport via MCT4 was sensitive to inhibition by the thiol reagent p-chloromercuribenzoesulphonic acid.


