WRW4Selective FPR2 antagonist CAS# 878557-55-2 |
- Tenovin-1
Catalog No.:BCC2239
CAS No.:380315-80-0
- HLI 373
Catalog No.:BCC2408
CAS No.:502137-98-6
- PRIMA-1
Catalog No.:BCC2413
CAS No.:5608-24-2
- Pifithrin-α (PFTα)
Catalog No.:BCC2241
CAS No.:63208-82-2
- NSC 319726
Catalog No.:BCC2242
CAS No.:71555-25-4
- JNJ-26854165 (Serdemetan)
Catalog No.:BCC2240
CAS No.:881202-45-5
Quality Control & MSDS
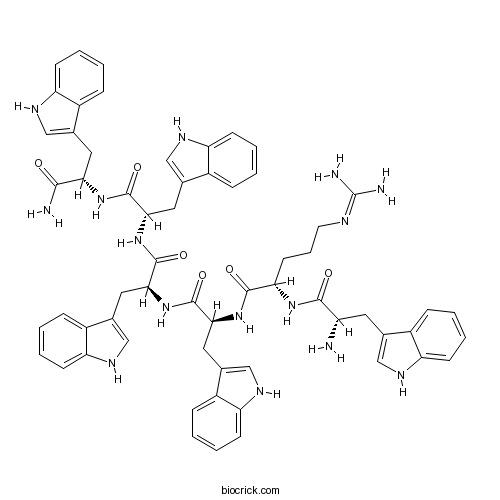
3D structure
Package In Stock
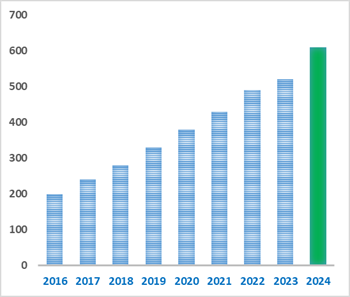
Number of papers citing our products
| Cas No. | 878557-55-2 | SDF | Download SDF |
| PubChem ID | 49768327 | Appearance | Powder |
| Formula | C61H65N15O6 | M.Wt | 1104.28 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Synonyms | WRW<sup>4</sup> | ||
| Solubility | Soluble to 1 mg/ml in water | ||
| Sequence | WRWWWW (Modifications: Trp-6 = C-terminal amide) | ||
| Chemical Name | (2S)-N-[(2S)-1-[[(2S)-1-[[(2S)-1-[[(2S)-1-amino-3-(1H-indol-3-yl)-1-oxopropan-2-yl]amino]-3-(1H-indol-3-yl)-1-oxopropan-2-yl]amino]-3-(1H-indol-3-yl)-1-oxopropan-2-yl]amino]-3-(1H-indol-3-yl)-1-oxopropan-2-yl]-2-[[(2S)-2-amino-3-(1H-indol-3-yl)propanoyl]amino]-5-(diaminomethylideneamino)pentanamide | ||
| SMILES | C1=CC=C2C(=C1)C(=CN2)CC(C(=O)NC(CCCN=C(N)N)C(=O)NC(CC3=CNC4=CC=CC=C43)C(=O)NC(CC5=CNC6=CC=CC=C65)C(=O)NC(CC7=CNC8=CC=CC=C87)C(=O)NC(CC9=CNC1=CC=CC=C19)C(=O)N)N | ||
| Standard InChIKey | IRJDOVLLPORVJP-WOAIKHIASA-N | ||
| Standard InChI | InChI=1S/C61H65N15O6/c62-44(24-34-29-67-45-17-6-1-12-39(34)45)56(78)72-50(22-11-23-66-61(64)65)57(79)74-53(27-37-32-70-48-20-9-4-15-42(37)48)59(81)76-54(28-38-33-71-49-21-10-5-16-43(38)49)60(82)75-52(26-36-31-69-47-19-8-3-14-41(36)47)58(80)73-51(55(63)77)25-35-30-68-46-18-7-2-13-40(35)46/h1-10,12-21,29-33,44,50-54,67-71H,11,22-28,62H2,(H2,63,77)(H,72,78)(H,73,80)(H,74,79)(H,75,82)(H,76,81)(H4,64,65,66)/t44-,50-,51-,52-,53-,54-/m0/s1 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Selective antagonist of formyl peptide receptor 2 (FPR2) signaling. Inhibits WKYMVm binding to FPR2 (IC50 = 0.23 μM) and inhibits intracellular calcium release induced by WKYMVm, MMK 1, amyloid β42, and F peptide. Also inhibits FPR2-mediated signaling in human neutrophils; blocks chemotactic migration and superoxide generation by amyloid β42 peptide. |

WRW4 Dilution Calculator

WRW4 Molarity Calculator
Calcutta University

University of Minnesota

University of Maryland School of Medicine
University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University
DRURY University
Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University
The University of Tokyo

Korea University
- JNJ 303
Catalog No.:BCC7806
CAS No.:878489-28-2
- Isosalviamine B
Catalog No.:BCN3554
CAS No.:878475-30-0
- Isosalviamine A
Catalog No.:BCN3553
CAS No.:878475-29-7
- Walrycin B
Catalog No.:BCC5156
CAS No.:878419-78-4
- Alismol
Catalog No.:BCN4427
CAS No.:87827-55-2
- S1RA
Catalog No.:BCC4189
CAS No.:878141-96-9
- Glucagon-like peptide 1 (1-37) (human, rat)
Catalog No.:BCC5827
CAS No.:87805-34-3
- 6beta-Hydroxyipolamiide
Catalog No.:BCN4426
CAS No.:87797-84-0
- TW-37
Catalog No.:BCC2257
CAS No.:877877-35-5
- erythro-Guaiacylglycerol beta-sinapyl ether
Catalog No.:BCN6605
CAS No.:877875-96-2
- Eupalinolide A
Catalog No.:BCN2524
CAS No.:877822-41-8
- Eupalinolide B
Catalog No.:BCN2525
CAS No.:877822-40-7
- Fostriecin sodium salt
Catalog No.:BCC2460
CAS No.:87860-39-7
- Lesinurad
Catalog No.:BCC1699
CAS No.:878672-00-5
- AZ 628
Catalog No.:BCC3730
CAS No.:878739-06-1
- 15-deoxy-Δ-12,14-Prostaglandin J2
Catalog No.:BCC7321
CAS No.:87893-55-8
- GDC-0449 (Vismodegib)
Catalog No.:BCC1285
CAS No.:879085-55-9
- CP 93129 dihydrochloride
Catalog No.:BCC6899
CAS No.:879089-64-2
- Psoracorylifol A
Catalog No.:BCN3611
CAS No.:879290-97-8
- Psoracorylifol B
Catalog No.:BCN7884
CAS No.:879290-98-9
- Psoracorylifol C
Catalog No.:BCN3708
CAS No.:879290-99-0
- 3,4,5-Tri-O-galloylquinic acid
Catalog No.:BCN8027
CAS No.:99745-62-7
- p-Hydroxyphenethyl anisate
Catalog No.:BCN6896
CAS No.:87932-34-1
- Prionoid B
Catalog No.:BCN3217
CAS No.:879324-75-1
Cathelicidin Suppresses Colon Cancer Metastasis via a P2RX7-Dependent Mechanism.[Pubmed:30847383]
Mol Ther Oncolytics. 2019 Jan 29;12:195-203.
The antimicrobial peptide cathelicidin inhibits development of colitis-associated colon cancer. However, the role of cathelicidin in colon cancer metastasis remains unknown. We hypothesized that cathelicidin is effective in inhibiting colon cancer metastasis. Human colon cancer HT-29 cells were injected intravenously into nude mice. Control HA-tagged adeno-associated virus (HA-AAV) or cathelicidin-overexpressing AAV (CAMP-HA-AAV) were injected intravenously into nude mice on the same day. Four weeks later, the nude mice were assessed for lung and liver metastases. Human colon cancer SW620 cells were used to study the effect of cathelicidin on cell migration and cytoskeleton. Incubation of SW620 cells with cathelicidin dose-dependently reduced cell migration, disrupted cytoskeletal structure, and reduced betaIII-tubulin (TUBB3) mRNA expression. The addition of the P2RX7 antagonist KN62, but not the FPRL1 antagonist WRW4, prevented the LL-37-mediated inhibition of cell migration and TUBB3 mRNA expression. The CAMP-HA-AAV-overexpressing group showed significantly reduced human CK20 protein (by 60%) and TUBB3 mRNA expression (by 40%) in the lungs and liver of the HT-29-loaded nude mice, compared to the HA-AAV control group. Intraperitoneal injection of KN62 reversed the CAMP-HA-AAV-mediated inhibition of human CK20 and TUBB3 expression in the lungs and liver of HT-29-loaded nude mice. In conclusion, cathelicidin inhibits colon cancer metastasis via a P2RX7-dependent pathway.
A long-lived peptide-conjugated iridium(iii) complex as a luminescent probe and inhibitor of the cell migration mediator, formyl peptide receptor 2.[Pubmed:30568767]
Chem Sci. 2018 Oct 1;9(43):8171-8177.
Formyl peptide receptors play important biological and therapeutic roles in wound repair and inflammatory diseases. In this work, we present a luminescent iridium(iii) complex (6) conjugated with the peptide agonist WKYMVm as a luminescent formyl peptide receptor 2 (FPR2) imaging probe in living cells. Complex 6 displayed ideal cell imaging characteristics, high photostability and low cytotoxicity. Competition assays with a known FPR2 antagonist, WRW4, and siRNA knockdown experiments both revealed that complex 6 selectively targeted FPR2 in living HUVEC cells. Moreover, complex 6 regulated FPR2 signalling in HUVEC cells as shown using a mechanical scratch assay. Finally, complex 6 reduced epithelial cell migration capacity and inhibited lipoxin A4 (LXA4)-triggered cell migration in HUVEC cells, demonstrating the ability of this complex to inhibit FPR2 in living cells. To our knowledge, this is the first long-lived probe for imaging FPR2 in living cells.
Activation of formyl peptide receptor 2 by WKYMVm enhances emergency granulopoiesis through phospholipase C activity.[Pubmed:30021674]
BMB Rep. 2018 Aug;51(8):418-423.
Emergency granulopoiesis is a very important strategy to supply efficient neutrophil number in response to infection. However, molecular mechanism involved in this process remains unclear. Here, we found that administration of WKYMVm, an immune modulating peptide, to septic mice strongly increased neutrophil number through augmented emergency granulopoiesis. WKYMVm-induced emergency granulopoiesis was blocked not only by a formyl peptide receptor 2 (FPR2) antagonist (WRW4), but also by FPR2 deficiency. As progenitors of neutrophils, Lin-c-kitSca-1- cells expressed FPR2. WKYMVm-induced emergency granulopoiesis was also blocked by a phospholipase C inhibitor (U-73122). These results suggest that WKYMVm can stimulate emergency granulopoiesis via FPR2 and phospholipase C enzymatic activity. [BMB Reports 2018; 51(8): 418-423].
Localisation of Formyl-Peptide Receptor 2 in the Rat Central Nervous System and Its Role in Axonal and Dendritic Outgrowth.[Pubmed:29948727]
Neurochem Res. 2018 Aug;43(8):1587-1598.
Arachidonic acid and docosahexaenoic acid (DHA) released by the action of phospholipases A2 (PLA2) on membrane phospholipids may be metabolized by lipoxygenases to the anti-inflammatory mediators lipoxin A4 (LXA4) and resolvin D1 (RvD1), and these can bind to a common receptor, formyl-peptide receptor 2 (FPR2). The contribution of this receptor to axonal or dendritic outgrowth is unknown. The present study was carried out to elucidate the distribution of FPR2 in the rat CNS and its role in outgrowth of neuronal processes. FPR2 mRNA expression was greatest in the brainstem, followed by the spinal cord, thalamus/hypothalamus, cerebral neocortex, hippocampus, cerebellum and striatum. The brainstem and spinal cord also contained high levels of FPR2 protein. The cerebral neocortex was moderately immunolabelled for FPR2, with staining mostly present as puncta in the neuropil. Dentate granule neurons and their axons (mossy fibres) in the hippocampus were very densely labelled. The cerebellar cortex was lightly stained, but the deep cerebellar nuclei, inferior olivary nucleus, vestibular nuclei, spinal trigeminal nucleus and dorsal horn of the spinal cord were densely labelled. Electron microscopy of the prefrontal cortex showed FPR2 immunolabel mostly in immature axon terminals or 'pre-terminals', that did not form synapses with dendrites. Treatment of primary hippocampal neurons with the FPR2 inhibitors, PBP10 or WRW4, resulted in reduced lengths of axons and dendrites. The CNS distribution of FPR2 suggests important functions in learning and memory, balance and nociception. This might be due to an effect of FPR2 in mediating arachidonic acid/LXA4 or DHA/RvD1-induced axonal or dendritic outgrowth.
The Annexin A1 Receptor FPR2 Regulates the Endosomal Export of Influenza Virus.[Pubmed:29738458]
Int J Mol Sci. 2018 May 8;19(5). pii: ijms19051400.
The Formyl Peptide Receptor 2 (FPR2) is a novel promising target for the treatment of influenza. During viral infection, FPR2 is activated by annexinA1, which is present in the envelope of influenza viruses; this activation promotes virus replication. Here, we investigated whether blockage of FPR2 would affect the genome trafficking of influenza virus. We found that, upon infection and cell treatment with the specific FPR2 antagonist WRW4 or the anti-FPR2 monoclonal antibody, FN-1D6-AI, influenza viruses were blocked into endosomes. This effect was independent on the strain and was observed for H1N1 and H3N2 viruses. In addition, blocking FPR2signaling in alveolar lung A549 epithelial cells with the monoclonal anti-FPR2 antibody significantly inhibited virus replication. Altogether, these results show that FPR2signaling interferes with the endosomal trafficking of influenza viruses and provides, for the first time, the proof of concept that monoclonal antibodies directed against FPR2 inhibit virus replication. Antibodies-based therapeutics have emerged as attractive reagents in infectious diseases. Thus, this study suggests that the use of anti-FPR2 antibodies against influenza hold great promise for the future.
Connections of annexin A1 and translocator protein-18kDa on toll like receptor stimulated BV-2 cells.[Pubmed:29649428]
Exp Cell Res. 2018 Jun 15;367(2):282-290.
BACKGROUND: Annexin A1 (ANXA1) and Translocator Protein-18KDa (TSPO) down-regulate neuroinflammation. We investigated the role of recombinant ANXA1 (rANXA) on TSPO functions on Toll Like Receptor (TLR) activated microglia. METHODS: BV-2 cells (murine microglia), were stimulated by E. coli Lipopolysaccharide (LPS) and treated with rANXA1 in order to measure TSPO expression and inflammatory parameters. Anti-sense ANXA1 and TLR4 and TSPO shRNA, as well as pharmacological treatments, were employed to assess the mechanisms involved. RESULTS: LPS-stimulated BV-2 cells caused overexpression of TSPO, which was inhibited by: pharmacological blockade of TLR4 or TLR4 mRNA silencing; inhibition of myeloid differentiation primary response gene 88 (MyD88) dimerization; or blocking of nuclear factor kappaB (NF-kappaB) activation. rANXA1 treatment impaired LPS-induced TSPO upregulation by down-modulating MyD88 and NF-kappaB signaling; the effect was abolished by WRW4, an antagonist of formyl peptide receptor 2 (FPR2). rANXA1 treatment also downregulated interleukin 1beta (IL-1beta) and tumor necrosis factor-alpha (TNFalpha) secretion in LPS-stimulated BV-2 cells. TSPO knockdown in BV-2 cells augmented LPS-induced TNFalpha secretion and abolished the inhibitory effect of rANXA1 on TNFalpha secretion evoked by LPS. CONCLUSIONS: exogenous ANXA1 down-modulates LPS-induced TSPO via MyD-88/NF-kappaB pathways, and constitutive TSPO is pivotal for the control of ANXA1 on TNFalpha secretion. TSPO actions may be involved with the mechanisms of ANXA1 on inflammatory brain diseases.
Resolvin D1 promotes corneal epithelial wound healing and restoration of mechanical sensation in diabetic mice.[Pubmed:29643724]
Mol Vis. 2018 Apr 1;24:274-285. eCollection 2018.
Purpose: To investigate the effect and mechanism of proresolving lipid mediator resolvin D1 (RvD1) on the corneal epithelium and the restoration of mechanical sensation in diabetic mice. Methods: Type 1 diabetes was induced in mice with intraperitoneal streptozocin injections. The healthy and diabetic mice underwent removal of the central corneal epithelium, and then 100 ng/ml RvD1 or its formyl peptide receptor 2 (FPR2) antagonist WRW4 was used to treat the diabetic mice. Regeneration of the corneal epithelium and nerves was observed with sodium fluorescein staining and whole-mount anti-beta3-tubulin fluorescence staining. The inflammatory response level was measured with hematoxylin and eosin staining (inflammatory cell infiltration), enzyme-linked immunosorbent assay (tumor necrosis factor alpha and interleukin-1 beta content), myeloperoxidase activity, and fluorescence staining (macrophage content). The reactive oxygen species (ROS) and glutathione (GSH) levels were examined with incubation with fluorescent probes, and oxidative stress-related protein expression levels were evaluated with fluorescence staining and western blotting. Results: Topical application of RvD1 promoted regeneration of the corneal epithelium in diabetic mice, accompanied by the reactivation of signaling and inflammation resolution related to regeneration of the epithelium. Furthermore, RvD1 directly attenuated the accumulation of ROS and nicotinamide adenine dinucleotide phosphate oxidase 2/4 expression, while RvD1 enhanced GSH synthesis and reactivated the Nrf2-ARE signaling pathway that was impaired in the corneal epithelium in the diabetic mice. More interestingly, topical application of RvD1 promoted regeneration of corneal nerves and completely restored impaired mechanical sensitivity of the cornea in diabetic mice. In addition, the promotion of corneal epithelial wound healing by RvD1 in diabetic mice was abolished by its FPR2 antagonist WRW4. Conclusions: Topical application of RvD1 promotes corneal epithelial wound healing and the restoration of mechanical sensation in diabetic mice, which may be related to the lipid mediator's regulation of inflammation resolution, the reactivation of regenerative signaling in the epithelium, and the attenuation of oxidative stress.
Inhibiting PSMalpha-induced neutrophil necroptosis protects mice with MRSA pneumonia by blocking the agr system.[Pubmed:29500427]
Cell Death Dis. 2018 Mar 2;9(3):362.
Given its high resistance, enhanced virulence, and high transmissibility, community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) pneumonia is highly associated with high morbidity and mortality. Anti-virulence therapy is a promising strategy that bypasses the evolutionary pressure on the bacterium to develop resistance. RNAIII-inhibiting peptide (RIP), as an accessory gene regulator (agr)-specific inhibitor, significantly restricts the virulence of S. aureus and protects infected mice from death by blocking the agr quorum sensing system. The protective effects of RIP on the neutropenic mice completely disappeared in a neutrophil-deleted mouse infection model, but not in the macrophage-deleted mice. This result confirmed that the in vivo antibacterial activity of RIP is highly associated with neutrophil function. Phenol-soluble modulins (PSMs), as major leukocyte lysis toxins of CA-MRSA, are directly regulated by the agr system. In this experiment, PSMalpha1, 2, and 3 significantly induced neutrophil necroptosis by activating mixed lineage kinase-like protein (MLKL) phosphorylation and increasing lactate dehydrogenase release. The S. aureus supernatants harvested from the agr or psmalpha mutant strains both decreased the phosphorylation level of MLKL and cell lysis. PSMalpha1-mediated neutrophil lysis was significantly inhibited by necrosulfonamide, necrostatin-1, TNFalpha antibody, and WRW4. These results showed PSMalpha1 induced necroptosis depends on formylpeptide receptor 2 (FPR2)-mediated autocrine TNFalpha. Moreover, the neutrophil necroptosis induced by S. aureus was significantly suppressed and pneumonia was effectively prevented by the blockage of agrA and psmalpha expression levels. These findings indicate that PSMalpha-induced necroptosis is a major cause of lung pathology in S. aureus pneumonia and suggest that interfering with the agr quorum sensing signaling pathway is a potential therapeutic strategy.
COOH-terminal SAA1 peptides fail to induce chemokines but synergize with CXCL8 and CCL3 to recruit leukocytes via FPR2.[Pubmed:29371208]
Blood. 2018 Jan 25;131(4):439-449.
A natural leukocyte chemoattractant was isolated from bovine serum by an established 4-step purification procedure. Based on its relative molecular mass of 7287 and NH2-terminal sequence, the protein was identified as a carboxy-terminal peptide of the acute phase protein serum amyloid A1 (SAA1). This SAA1(46-112) fragment and its human equivalent SAA1(47-104) were chemically synthesized. Unlike intact SAA1alpha, these SAA fragments failed to directly chemoattract neutrophils and monocytes, to induce chemokines, and to stimulate downstream extracellular signal-regulated kinase signaling in monocytes. However, the SAA fragments potently synergized with CCL3 to induce monocyte migration and with CXCL8 to stimulate neutrophil shape changes and chemotaxis. Unlike intact SAA1alpha, SAA1(46-112) did not induce CXCL6 ex vivo but provoked a cooperative intraperitoneal neutrophil recruitment in mice when coinjected with CXCL6 into the peritoneal cavity. Moreover, SAA1(47-104) desensitized the synergy between intact SAA1alpha and CXCL8 in neutrophil chemotaxis, suggesting that this peptide binds formyl peptide receptor 2 (FPR2). This was evidenced by a complete blockade of synergy between the COOH-terminal SAA1 fragments and CXCL8 or CCL3 in neutrophil and monocyte chemotaxis, respectively, by the FPR2 antagonist WRW4 Thus, SAA1 is degraded into fragments lacking chemokine-inducing capacity, while keeping synergy with cytokine-induced chemokines to sustain limited inflammation.
COOH-terminal SAA1 peptides fail to induce chemokines but synergize with CXCL8 and CCL3 to recruit leukocytes via FPR2.[Pubmed:29203586]
Blood. 2017 Dec 4. pii: blood-2017-06-788554.
A natural leukocyte chemoattractant was isolated from bovine serum by an established four-step purification procedure. Based on its relative molecular mass of 7287 and NH2-terminal sequence, the protein was identified as a carboxy-terminal peptide of the acute phase protein serum amyloid A (SAA) 1. This SAA1(46-112) fragment and its human equivalent SAA1(47-104) were chemically synthesized. Unlike intact SAA1alpha, these SAA fragments failed to directly chemoattract neutrophils and monocytes, to induce chemokines and to stimulate downstream ERK signaling in monocytes. However, the SAA fragments potently synergized with CCL3 to induce monocyte migration and with CXCL8 to stimulate neutrophil shape change and chemotaxis. Unlike intact SAA1alpha, SAA1(46-112) did not induce CXCL6 ex vivo, but provoked a cooperative intraperitoneal neutrophil recruitment in mice when co-injected with CXCL6 into the peritoneal cavity. Moreover, SAA1(47-104) desensitized the synergy between intact SAA1alpha and CXCL8 in neutrophil chemotaxis, suggesting that this peptide binds formyl peptide receptor (FPR) 2. This was evidenced by a complete blockade of synergy between the COOH-terminal SAA1 fragments and CXCL8 or CCL3 in neutrophil and monocyte chemotaxis, respectively, by the FPR2 antagonist WRW4 Thus, SAA1 is degraded into fragments lacking chemokine-inducing capacity, whilst keeping synergy with cytokine-induced chemokines to sustain limited inflammation.
FAM19A5, a brain-specific chemokine, inhibits RANKL-induced osteoclast formation through formyl peptide receptor 2.[Pubmed:29138422]
Sci Rep. 2017 Nov 14;7(1):15575.
Osteoclasts can be differentiated from bone marrow-derived macrophages (BMDM). They play a key role in bone resorption. Identifying novel molecules that can regulate osteoclastogenesis has been an important issue. In this study, we found that FAM19A5, a neurokine or brain-specific chemokine, strongly stimulated mouse BMDM, resulting in chemotactic migration and inhibition of RANKL-induced osteoclastogenesis. Expression levels of osteoclast-related genes such as RANK, TRAF6, OSCAR, TRAP, Blimp1, c-fos, and NFATc1 were markedly decreased by FAM19A5. However, negative regulators of osteoclastogenesis such as MafB and IRF-8 were upregulated by FAM19A5. FAM19A5 also downregulated expression levels of RANKL-induced fusogenic genes such as OC-STAMP, DC-STAMP, and Atp6v0d2. FAM19A5-induced inhibitory effect on osteoclastogenesis was significantly reversed by a formyl peptide receptor (FPR) 2 antagonist WRW4 or by FPR2-deficiency, suggesting a crucial role of FPR2 in the regulation of osteoclastogenesis. Collectively, our results suggest that FAM19A5 and its target receptor FPR2 can act as novel endogenous ligand/receptor to negatively regulate osteoclastogenesis. They might be regarded as potential targets to control osteoclast formation and bone disorders.
Lipoxin A4 encapsulated in PLGA microparticles accelerates wound healing of skin ulcers.[Pubmed:28753648]
PLoS One. 2017 Jul 28;12(7):e0182381.
Lipoxin A4 (LXA4) is involved in the resolution of inflammation and wound healing; however, it is extremely unstable. Thus, to preserve its biological activities and confer stability, we encapsulated LXA4 in poly-lactic-co-glycolic acid (PLGA) microparticles (LXA4-MS) and assessed its application in treating dorsal rat skin lesions. Ulcers were sealed with fibrin adhesive and treated with either LXA4-MS, unloaded microparticles (Un-MS), soluble LXA4, or PBS/glue (vehicle). All groups were compared at 0, 2, 7, and 14 days post-lesions. Our results revealed that LXA4-MS accelerated wound healing from day 7 and reduced initial ulcer diameters by 80%. Soluble LXA4, Un-MS, or PBS closed wounds by 60%, 45%, and 39%, respectively. LXA4-MS reduced IL-1beta and TNF-alpha, but increased TGF-beta, collagen deposition, and the number of blood vessels. Compared to other treatments, LXA4-MS reduced inflammatory cell numbers, myeloperoxidase (MPO) concentration, and metalloproteinase-8 (MMP8) mRNA in scar tissue, indicating decreased neutrophil chemotaxis. In addition, LXA4-MS treatment increased macrophages and IL-4, suggesting a positive impact on wound healing. Finally, we demonstrated that WRW4, a selective LXA4 receptor (ALX) antagonist, reversed healing by 50%, indicating that LXA4 must interact with ALX to induce wound healing. Our results show that LXA4-MS could be used as a pharmaceutical formulation for the treatment of skin ulcers.
Mast cells mediate early neutrophil recruitment and exhibit anti-inflammatory properties via the formyl peptide receptor 2/lipoxin A4 receptor.[Pubmed:28471519]
Br J Pharmacol. 2017 Jul;174(14):2393-2408.
BACKGROUND AND PURPOSE: In recent years, studies have focused on the resolution of inflammation, which can be achieved by endogenous anti-inflammatory agonists such as Annexin A1 (AnxA1). Here, we investigated the effects of mast cells (MCs) on early LPS-induced neutrophil recruitment and the involvement of the AnxA1-formyl peptide receptor 2/ALX (FPR2/ALX or lipoxin A4 receptor) pathway. EXPERIMENTAL APPROACH: Intravital microscopy (IVM) was used to visualize and quantify the effects of LPS (10 mug per mouse i.p.) on murine mesenteric cellular interactions. Furthermore, the role that MCs play in these inflammatory responses was determined in vivo and in vitro, and effects of AnxA1 mimetic peptide Ac2-26 were assessed. KEY RESULTS: LPS increased both neutrophil endothelial cell interactions within the mesenteric microcirculation and MC activation (determined by IVM and ruthenium red dye uptake), which in turn lead to the early stages of neutrophil recruitment. MC recruitment of neutrophils could be blocked by preventing the pro-inflammatory activation (using cromolyn sodium) or enhancing an anti-inflammatory phenotype (using Ac2-26) in MCs. Furthermore, MCs induced neutrophil migration in vitro, and MC stabilization enhanced the release of AnxA1 from neutrophils. Pharmacological approaches (such as the administration of FPR pan-antagonist Boc2, or the FPR2/ALX antagonist WRW4) revealed neutrophil FPR2/ALX to be important in this process. CONCLUSIONS AND IMPLICATIONS: Data presented here provide evidence for a role of MCs, which are ideally positioned in close proximity to the vasculature, to act as sentinel cells in neutrophil extravasation and resolution of inflammation via the AnxA1-FPR2/ALX pathway.
Resolvin D1 and D2 Reverse Lipopolysaccharide-Induced Depression-Like Behaviors Through the mTORC1 Signaling Pathway.[Pubmed:28419244]
Int J Neuropsychopharmacol. 2017 Jul 1;20(7):575-584.
Background: Resolvin D1 and D2 are bioactive lipid mediators that are generated from docosahexaenoic acid. Although recent preclinical studies suggest that these compounds have antidepressant effects, their mechanisms of action remain unclear. Methods: We investigated mechanisms underlying the antidepressant effects of resolvin D1 and resolvin D2 in lipopolysaccharide (0.8 mg/kg, i.p.)-induced depression model mice using a tail suspension test. Results: I.c.v. infusion of resolvin D1 (10 ng) and resolvin D2 (10 ng) produced antidepressant effects; these effects were significantly blocked by a resolvin D1 receptor antagonist WRW4 (10 microg, i.c.v.) and a resolvin D2 receptor antagonist O-1918 (10 microg, i.c.v.), respectively. The mammalian target of rapamycin complex 1 inhibitor rapamycin (10 mg/kg, i.p.) and a mitogen-activated protein kinase kinase inhibitor U0126 (5 microg, i.c.v.) significantly blocked the antidepressant effects of resolvin D1 and resolvin D2. An AMPA receptor antagonist NBQX (10 mg/kg, i.p.) and a phosphoinositide 3-kinase inhibitor LY294002 (3 microg, i.c.v.) blocked the antidepressant effects of resolvin D1 significantly, but not of resolvin D2. Bilateral infusions of resolvin D1 (0.3 ng/side) or resolvin D2 (0.3 ng/side) into the medial prefrontal cortex or dentate gyrus of the hippocampus produced antidepressant effects. Conclusions: These findings demonstrate that resolvin D1 and resolvin D2 produce antidepressant effects via the mammalian target of rapamycin complex 1 signaling pathway, and that the medial prefrontal cortex and dentate gyrus are important brain regions for these antidepressant effects. These compounds and their receptors may be promising targets for the development of novel rapid-acting antidepressants, like ketamine and scopolamine.
Hydroalcoholic crude extract of Casearia sylvestris Sw. reduces chronic post-ischemic pain by activation of pro-resolving pathways.[Pubmed:28412216]
J Ethnopharmacol. 2017 May 23;204:179-188.
ETHNOPHARMACOLOGICAL RELEVANCE: Casearia sylvestris Sw. is widely used in popular medicine to treat conditions associated with pain. AIM OF THE STUDY: The present study investigated the influence of hydroalcoholic crude extract of Casearia sylvestris (HCE-CS) and contribution of pro-resolving mediators on mechanical hyperalgesia in a mouse model of chronic post-ischemia pain (CPIP). METHODS AND RESULTS: Male Swiss mice were subjected to ischemia of the right hind paw (3h), then reperfusion was allowed. At 10min, 24h or 48h post-ischemia/reperfusion (I/R), different groups of animals were treated with HCE-CS (30mg/Kg, orally [p.o]), selected agonists at the pro-resolving receptor ALX/FPR2 (natural molecules like resolvin D1 and lipoxin A4 or the synthetic compound BML-111; 0.1-1microg/animal) or vehicle (saline, 10mL/Kg, s.c.), in the absence or presence of the antagonist WRW4 (10microg, s.c.). Mechanical hyperalgesia (paw withdrawal to von Frey filament) was asseseed together with histological and immunostainning analyses. In these settings, pro-resolving mediators reduced mechanical hyperalgesia and HCE-CS or BML-111 displayed anti-hyperalgesic effects which was markedly attenuated in animals treated with WRW4. ALX/FPR2 expression was raised in skeletal muscle or neutrophils after treatment with HCE-CS or BML-111. CONCLUSION: These results reveal significant antihyperalgesic effect of HCE-CS on CPIP, mediated at least in part, by the pathway of resolution of inflammation centred on the axis modulated by ALX/FPR2.
Identification of peptides that antagonize formyl peptide receptor-like 1-mediated signaling.[Pubmed:15210823]
J Immunol. 2004 Jul 1;173(1):607-14.
Formyl peptide receptor-like 1 (FPRL1) is an important classical chemoattractant receptor that is expressed in phagocytic cells in the peripheral blood and brain. Recently, various novel agonists have been identified from several origins, such as host-derived molecules. Activation of FPRL1 is closely related to inflammatory responses in the host defense mechanism and neurodegenerative disorders. In the present study we identified several novel peptides by screening hexapeptide libraries that inhibit the binding of one of FPRL1's agonists (Trp-Lys-Tyr-Met-Val-D-Met-CONH(2) (WKYMVm)) to its specific receptor, FPRL1, in RBL-2H3 cells. Among the novel peptides, Trp-Arg-Trp-Trp-Trp-Trp-CONH(2) (WRWWWW (WRW(4))) showed the most potent activity in terms of inhibiting WKYMVm binding to FPRL1. We also found that WRW(4) inhibited the activation of FPRL1 by WKYMVm, resulting in the complete inhibition of the intracellular calcium increase, extracellular signal-regulated kinase activation, and chemotactic migration of cells toward WKYMVm. For the receptor specificity of WRW(4) to the FPR family, we observed that WRW(4) specifically inhibit the increase in intracellular calcium by the FPRL1 agonists MMK-1, amyloid beta42 (Abeta42) peptide, and F peptide, but not by the FPR agonist, fMLF. To investigate the effect of WRW(4) on endogenous FPRL1 ligand-induced cellular responses, we examined its effect on Abeta42 peptide in human neutrophils. Abeta42 peptide-induced superoxide generation and chemotactic migration of neutrophils were inhibited by WRW(4), which also completely inhibited the internalization of Abeta42 peptide in human macrophages. WRW(4) is the first specific FPRL1 antagonist and is expected to be useful in the study of FPRL1 signaling and in the development of drugs against FPRL1-related diseases.


