DoxercalciferolVitamin D receptor activator CAS# 54573-75-0 |

- Salmefamol
Catalog No.:BCC1919
CAS No.:18910-65-1
- Guanfacine hydrochloride
Catalog No.:BCC1609
CAS No.:29110-48-3
- (R,R)-Formoterol
Catalog No.:BCC1293
CAS No.:67346-49-0
- Medetomidine
Catalog No.:BCC1736
CAS No.:86347-14-0
Quality Control & MSDS
3D structure
Package In Stock
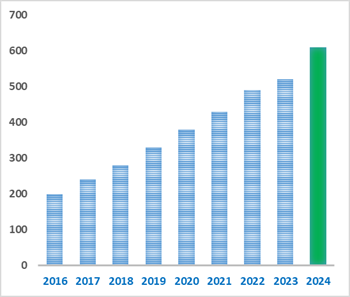
Number of papers citing our products
| Cas No. | 54573-75-0 | SDF | Download SDF |
| PubChem ID | 5281107 | Appearance | Powder |
| Formula | C28H44O2 | M.Wt | 412.66 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Synonyms | 1.alpha.-Hydroxyvitamin D2 | ||
| Solubility | DMSO : ≥ 50 mg/mL (121.17 mM) H2O : < 0.1 mg/mL (insoluble) *"≥" means soluble, but saturation unknown. | ||
| Chemical Name | (1R,3S,5Z)-5-[(2E)-2-[(1R,3aS,7aR)-1-[(E,2R,5R)-5,6-dimethylhept-3-en-2-yl]-7a-methyl-2,3,3a,5,6,7-hexahydro-1H-inden-4-ylidene]ethylidene]-4-methylidenecyclohexane-1,3-diol | ||
| SMILES | CC(C)C(C)C=CC(C)C1CCC2C1(CCCC2=CC=C3CC(CC(C3=C)O)O)C | ||
| Standard InChIKey | HKXBNHCUPKIYDM-CGMHZMFXSA-N | ||
| Standard InChI | InChI=1S/C28H44O2/c1-18(2)19(3)9-10-20(4)25-13-14-26-22(8-7-15-28(25,26)6)11-12-23-16-24(29)17-27(30)21(23)5/h9-12,18-20,24-27,29-30H,5,7-8,13-17H2,1-4,6H3/b10-9+,22-11+,23-12-/t19-,20+,24+,25+,26-,27-,28+/m0/s1 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Vitamin D2 analog that acts as a vitamin D receptor activator (VDRA). |

Doxercalciferol Dilution Calculator

Doxercalciferol Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 2.4233 mL | 12.1165 mL | 24.233 mL | 48.466 mL | 60.5826 mL |
| 5 mM | 0.4847 mL | 2.4233 mL | 4.8466 mL | 9.6932 mL | 12.1165 mL |
| 10 mM | 0.2423 mL | 1.2117 mL | 2.4233 mL | 4.8466 mL | 6.0583 mL |
| 50 mM | 0.0485 mL | 0.2423 mL | 0.4847 mL | 0.9693 mL | 1.2117 mL |
| 100 mM | 0.0242 mL | 0.1212 mL | 0.2423 mL | 0.4847 mL | 0.6058 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||
Calcutta University

University of Minnesota

University of Maryland School of Medicine
University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University
DRURY University
Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University
The University of Tokyo

Korea University
Doxercalciferol (Hectorol; 1.alpha.-Hydroxyvitamin D2) is a synthetic analog of vitamin D. Doxercalciferol (Hectorol; 1.alpha.-Hydroxyvitamin D2) is a Vitamin D2 analog that acts as a vitamin D receptor activator (VDRA).
- Quercetin-3-O-glucose-6'-acetate
Catalog No.:BCN6545
CAS No.:54542-51-7
- AMG 9810
Catalog No.:BCC7329
CAS No.:545395-94-6
- QNZ (EVP4593)
Catalog No.:BCC2249
CAS No.:545380-34-5
- Nicardipine HCl
Catalog No.:BCC4685
CAS No.:54527-84-3
- Methyl protogracillin
Catalog No.:BCN8177
CAS No.:54522-53-1
- Methyl protodioscin
Catalog No.:BCN6342
CAS No.:54522-52-0
- H-Leu-CMK.HCl
Catalog No.:BCC2971
CAS No.:54518-92-2
- 5-Aminolevulinic acid HCl
Catalog No.:BCC4883
CAS No.:5451-09-2
- Erythrodiol
Catalog No.:BCN5726
CAS No.:545-48-2
- Lupeol
Catalog No.:BCN5725
CAS No.:545-47-1
- Uvaol
Catalog No.:BCN5724
CAS No.:545-46-0
- 5-Glutinen-3-ol
Catalog No.:BCN5723
CAS No.:545-24-4
- Conessine
Catalog No.:BCC7352
CAS No.:546-06-5
- Alantolactone
Catalog No.:BCN1033
CAS No.:546-43-0
- α-Thujone
Catalog No.:BCC8271
CAS No.:546-80-5
- Columbin
Catalog No.:BCN2622
CAS No.:546-97-4
- Boc-Lys(2-Cl-Z)-OH
Catalog No.:BCC3416
CAS No.:54613-99-9
- URB597
Catalog No.:BCC2324
CAS No.:546141-08-6
- Diethyl 2-acetamido-2-phenethylmalonate
Catalog No.:BCC8940
CAS No.:5463-92-3
- Boc-Hyp(Bzl)-OH.DCHA
Catalog No.:BCC3253
CAS No.:54631-81-1
- 2-Amino-4-methoxybenzothiazole
Catalog No.:BCC8532
CAS No.:5464-79-9
- ML 204
Catalog No.:BCC6272
CAS No.:5465-86-1
- 1-O-Methyljatamanin D
Catalog No.:BCN6671
CAS No.:54656-47-2
- 2-(Acetylamino)-3-phenyl-2-propenoic acid
Catalog No.:BCN1420
CAS No.:5469-45-4
Involvement of microRNA181a in differentiation and cell cycle arrest induced by a plant-derived antioxidant carnosic acid and vitamin D analog doxercalciferol in human leukemia cells.[Pubmed:25048087]
Microrna. 2012;1(1):26-33.
1,25-dihydroxyvitamin D3 (1,25D) has been shown to influence differentiation, cell proliferation and cell death in cultured leukemia cells. However, its clinical use is limited by its hypercalcemic effects. An analog of 1,25D, Doxercalciferol (1-D2), has anti-tumor activity, with markedly reduced calcemic effects, which makes it a potential agent for clinical treatment of AML. Previous studies suggested that the combination of 1,25D with other agents, such as plant-derived antioxidants, can have additive or synergistic anti-cancer activities in leukemia cells. Here we report that 1-D2 induced monocytic differentiation of HL60 and U937 cells, and that the antioxidant carnosic acid (CA) enhanced 1-D2 induced differentiation and cell cycle arrest. MicroRNA181a (miR181a) expression was also reduced after exposure to CA/1-D2. Since the cell cycle regulator p27Kip1 has been shown to be a target of miR181a, we modulated miR181a levels to determine if it plays a role in CA/1-D2 induced differentiation and cell cycle arrest in AML cells. We found that transfection of antisense miR181a potentiated CA/1-D2-induced cell differentiation, while the transfection of precursor of miR181a partially inhibited the effect of CA/1-D2 on the differentiation. These findings imply that miR181a has a role in CA/1-D2- induced differentiation and cell cycle arrest of HL60 and U937 cells, and shows a broader participation of miR181a in cell cycle control in leukemia cells.
Determination of degradation products of doxercalciferol by solid-phase extraction and reversed-phase HPLC.[Pubmed:23780943]
J Chromatogr Sci. 2014 Jul;52(6):520-5.
In the current study, injectable formulations containing Doxercalciferol as the active pharmaceutical ingredient are analyzed by using gradient-elution high-performance liquid chromatography with ultraviolet detection. Various related impurities and degradants are quantified by using solid-phase extraction (SPE) for enhanced sensitivity. The assay of possible related impurities and Doxercalciferol analogues present at trace quantities is performed by using Trans-1-alpha-hydroxy vitamin D2 (Doxercalciferol related degradation product/Impurity B) as standard and 1-beta-hydroxy vitamin D2 (Doxercalciferol related degradation product/Impurity C) as internal standards for the SPE study. The current method is shown to be stability-indicating and free from interferences from any of the formulation excipients and potential degradation products and impurities. The validated method is shown to be reproducible, accurate, sensitive and selective.
Osteocytic protein expression response to doxercalciferol therapy in pediatric dialysis patients.[Pubmed:25774916]
PLoS One. 2015 Mar 16;10(3):e0120856.
BACKGROUND: Osteocytic protein expression is dysregulated in CKD and is affected by changes in mineral metabolism; however the effects of active vitamin D sterol therapy on osteocyte protein expression in advanced CKD is unknown. METHODS: Eleven pediatric patients with end stage kidney disease underwent bone biopsy, were treated for 8 months with Doxercalciferol, and then underwent a second bone biopsy. Bone expression of fibroblast growth factor 23 (FGF23), dentin matrix protein 1 (DMP1), and sclerostin were determined by immunohistochemistry and quantified by Ariol Scanning. Western blot analysis and qRT-PCR was performed on bone abstracts of a subset of study subjects to determine the nature (i.e. size) of FGF23 and DMP1 in bone before and after therapy. RESULTS: As assessed by immunohistochemistry, bone FGF23, DMP1 and sclerostin protein all increased with therapy. In the case of FGF23, this increase was due to an increase in the full-length molecule without the appearance of FGF23 fragments. DMP1 was present primarily in its full-length form in healthy controls while 57kDa and 37kDa fragments of DMP1 were apparent in bone of dialysis patients at baseline and the 57 kDa appeared to decrease with therapy. CONCLUSION: Marked changes in osteocytic protein expression accompany Doxercalciferol therapy, potentially impacting bone mineralization and the skeletal response to PTH. The effects of these bone changes on long-term outcomes remain to be determined.
Efficacy and safety of oral doxercalciferol in the management of secondary hyperparathyroidism in chronic kidney disease stage 4.[Pubmed:23960343]
Indian J Nephrol. 2013 Jul;23(4):271-5.
This study was carried out to evaluate the efficacy and safety of Doxercalciferol as therapy for secondary hyperparathyroidism (SHPT) in patients with chronic kidney disease (CKD) stage 4 in a prospective clinical trial. A total of 35 CKD-4 patients who had a baseline parathyroid hormone (iPTH) >150 pg/mL and had not received any vitamin D analog in the preceding 8 weeks were followed up at intervals of 6 weeks for 18 weeks on oral therapy with Doxercalciferol. The starting dose was 1.5 mug/day, and the dose was increased in steps of 1 mug/day if iPTH did not decrease by at least 30% on the subsequent visit. Doxercalciferol was stopped temporarily if low iPTH (<70 pg/mL), hypercalcemia (>10.7 mg/dL), or severe hyperphosphatemia (>8.0 mg/dL) occurred, and was restarted at a lower dose on reversal of these abnormalities. Calcium acetate was the only phosphate binder used. Mean iPTH decreased by 35.4 +/- 4.4% from 381.7 +/- 31.3 pg/mL to 237.9 +/- 25.7 pg/mL (P < 0.001). The proportion of patients who achieved 30% and 50% suppression of iPTH levels was 83% and 72%, respectively. Mean serum calcium, phosphorus, and calcium-phosphorus product values did not differ significantly from the baseline values. Four, two, and nine patients developed hypercalcemia, severe hyperphosphatemia, and high CaxP (>55), respectively. Almost all patients recovered to an acceptable level within 2 weeks of stopping Doxercalciferol and adjusting the phosphate binder dose. In all, 21 patients required temporary stoppage of therapy. Most of them were restarted on therapy at a reduced dose during the study. It can, therefore, be concluded that Doxercalciferol is effective in controlling SHPT in CKD-4 patients with an acceptable risk of hyperphosphatemia and hypercalcemia.
Differential effects of vitamin D receptor activators on aortic calcification and pulse wave velocity in uraemic rats.[Pubmed:18644798]
Nephrol Dial Transplant. 2008 Dec;23(12):3824-30.
BACKGROUND: Vascular calcification is associated with an increase in cardiovascular mortality in stage 5 chronic kidney disease. To determine if vitamin D receptor activators (VDRAs) have differential effects in the pathogenesis of aortic calcification, we assessed the effects of paricalcitol and Doxercalciferol in vivo using 5/6 nephrectomized (NX) rats. To quantify the functional consequences of vascular calcification, pulse wave velocity (PWV), an aortic compliance index, was measured. METHODS: NX rats were fed a diet containing 0.9% phosphorous and 0.6% calcium 4 weeks prior to and throughout the study. On Day 0, rats received vehicle or VDRA (0.083, 0.167 and 0.333 microg/kg, i.p.) three times per week for 6 weeks. At Day 0 and Weeks 2 and 6, blood was drawn and PWV was measured by Doppler ultrasound. RESULTS: VDRAs (0.167 and 0.333 microg/kg) consistently lowered PTH at Weeks 2 and 6. All doses of paricalcitol increased serum calcium at Week 6 but not at Week 2, while the two higher doses of Doxercalciferol increased serum calcium at both Weeks 2 and 6. Treatment with paricalcitol (0.333 microg/kg) increased serum phosphorus at Weeks 2 and 6; these changes were not different from those observed in 5/6 NX rats. All doses of Doxercalciferol increased serum phosphorus at Week 6. Paricalcitol had no effect on Ca x P; however, the two highest doses of Doxercalciferol increased Ca x P at Weeks 2 and 6 above that observed in the 5/6 NX vehicle-treated group. There were no differences in aortic calcium and phosphorus contents at the end of 6 weeks among SHAM-, 5/6 NX- and paricalcitol-treated rats. However, treatment with the two higher doses of Doxercalciferol caused a significant elevation in aortic calcium and phosphorus contents. Measurements of PWV demonstrated differential effects of VDRAs on vascular compliance. Paricalcitol produced no effects on PWV, while the two highest doses of Doxercalciferol increased PWV at Week 6. CONCLUSIONS: In uraemic rats with established secondary hyperparathyroidism, we demonstrate differential effects of paricalcitol and Doxercalciferol on aortic calcification and PWV, independent of serum Ca, P and Ca x P, suggesting different mechanisms of action between VDRAs.
The vitamin D prodrugs 1alpha(OH)D2, 1alpha(OH)D3 and BCI-210 suppress PTH secretion by bovine parathyroid cells.[Pubmed:16221703]
Nephrol Dial Transplant. 2006 Mar;21(3):644-50.
BACKGROUND: Active vitamin D compounds are widely used in the treatment of secondary hyperparathyroidism associated with renal failure. These compounds reduce PTH secretion through vitamin D receptor (VDR)-dependent repression of PTH gene transcription. In previous studies, 1alpha(OH)D3, a vitamin D prodrug, inhibited PTH secretion in cultured bovine parathyroid cells, but it was unclear whether 1alpha(OH)D3 itself or an active metabolite produced this inhibition. METHODS: We determined the effectiveness of the vitamin D prodrugs 1alpha(OH)D3, 1alpha(OH)D2 and 1alpha(OH)-24(R)-methyl-25-ene-D2 (BCI-210) at inhibiting PTH secretion in bovine parathyroid cell cultures, and examined the metabolism of [3H]1alpha(OH)D2 in these cells. RESULTS: All three prodrugs suppressed PTH secretion with approximately 10% of the activity of 1,25(OH)2D3; much higher activity than expected based on the VDR affinities of these prodrugs (0.25% of 1,25(OH)2D3). Parathyroid cells activated [3H]1alpha(OH)D2 to both 1,25(OH)2D2 and 1,24(OH)2D2. 1,24(OH)2D2 was detectable at 4 h, increased to a maximum at 8 h, and then decreased. In contrast, 1,25(OH)2D2 levels increased linearly with time, suggesting the presence of constitutively active vitamin D-25-hydroxylase not previously reported in parathyroid cells. The cytochrome P-450 inhibitor ketoconazole (50 microM) reduced 1alpha(OH)D2 metabolism to below detectable levels, but did not significantly affect suppression of PTH by 1alpha(OH)D2. CONCLUSIONS: The vitamin D prodrugs 1alpha(OH)D3, 1alpha(OH)D2 and BCI-210 suppressed PTH production by cultured parathyroid cells. The ability of 1alpha(OH)D2 to reduce PTH despite inhibition of its metabolism suggests a direct action of this 'prodrug' on the parathyroid gland, but the mechanism underlying this activity is not yet known.


