FurosemideGABAA receptors antagonist CAS# 54-31-9 |
- Bumetanide
Catalog No.:BCC1119
CAS No.:28395-03-1
Quality Control & MSDS
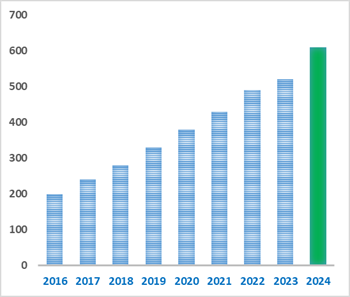
Number of papers citing our products
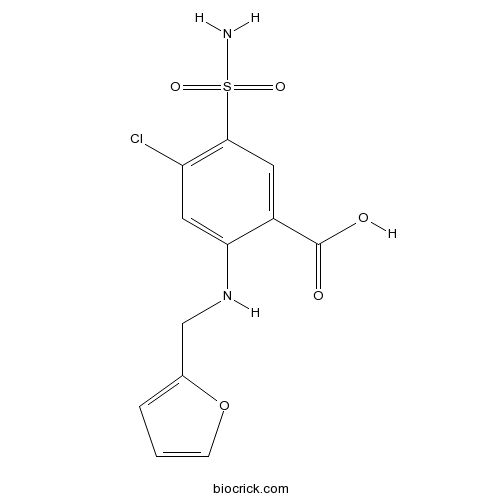
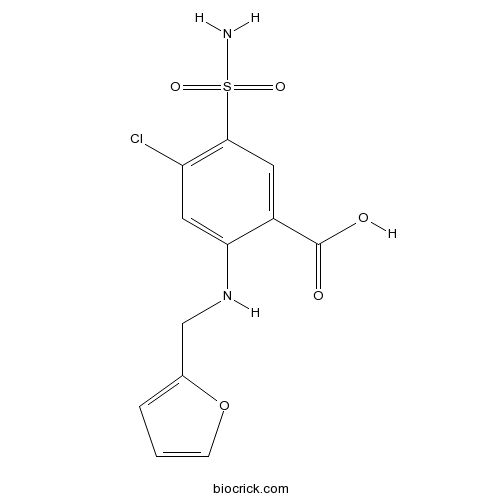
Chemical structure
3D structure
| Cas No. | 54-31-9 | SDF | Download SDF |
| PubChem ID | 3440 | Appearance | Powder |
| Formula | C12H11ClN2O5S | M.Wt | 330.74 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | DMSO : ≥ 100 mg/mL (302.35 mM) H2O : < 0.1 mg/mL (insoluble) *"≥" means soluble, but saturation unknown. | ||
| Chemical Name | 4-chloro-2-(furan-2-ylmethylamino)-5-sulfamoylbenzoic acid | ||
| SMILES | C1=COC(=C1)CNC2=CC(=C(C=C2C(=O)O)S(=O)(=O)N)Cl | ||
| Standard InChIKey | ZZUFCTLCJUWOSV-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C12H11ClN2O5S/c13-9-5-10(15-6-7-2-1-3-20-7)8(12(16)17)4-11(9)21(14,18)19/h1-5,15H,6H2,(H,16,17)(H2,14,18,19) | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Loop diuretic that inhibits the Na+/2Cl-/K+ (NKCC) symporter. Also acts as a non-competitive antagonist at GABAA receptors with ~ 100-fold greater selectivity for α6-containing receptors than α1-containing receptors. |

Furosemide Dilution Calculator

Furosemide Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 3.0235 mL | 15.1176 mL | 30.2352 mL | 60.4705 mL | 75.5881 mL |
| 5 mM | 0.6047 mL | 3.0235 mL | 6.047 mL | 12.0941 mL | 15.1176 mL |
| 10 mM | 0.3024 mL | 1.5118 mL | 3.0235 mL | 6.047 mL | 7.5588 mL |
| 50 mM | 0.0605 mL | 0.3024 mL | 0.6047 mL | 1.2094 mL | 1.5118 mL |
| 100 mM | 0.0302 mL | 0.1512 mL | 0.3024 mL | 0.6047 mL | 0.7559 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||
Calcutta University

University of Minnesota

University of Maryland School of Medicine
University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University
DRURY University
Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University
The University of Tokyo

Korea University
Furosemide is an inhibitor of Na+/2Cl-/K+ cotransporter [1].
The Na-K-Cl cotransporter (NKCC) is a protein that acts as an active transporter helping sodium, potassium, and chloride into and out of cells. NKCC1 has important functions in organs that secrete fluids. NKCC2 exists in the kidney and serves to extract sodium, potassium, and chloride from the urine [2].
Furosemide is an antagonist of Na+/2Cl-/K+ cotransporter. In adult brain tissue, furosemide blocked the epileptiform activity through inhibiting cell swelling, which was concomitant with its inhibition of activity-driven changes of the extracellular space (ECS) [1]. Furosemide inhibited the production and release of cytokines IL-6, IL-8, and TNF-ɑ from peripheral mononuclear cells and exhibited an anti-inflammatory effect [3].
In patients with liver cirrhosis, furosemide inhibited the natriuretic effect and increased the levels of atrial natriuretic factor (ANF) and circulating endothelin. In neonates, furosemide significantly increased the urinary excretion of aldosterone and endothelin-1 [3].
References:
[1]. Hochman DW. The extracellular space and epileptic activity in the adult brain: explaining the antiepileptic effects of furosemide and bumetanide. Epilepsia, 2012, 53 Suppl 1: 18-25.
[2]. Chen H, Sun D. The role of Na-K-Cl co-transporter in cerebral ischemia. Neurol Res, 2005, 27(3): 280-286.
[3]. Prandota J. Furosemide: progress in understanding its diuretic, anti-inflammatory, and bronchodilating mechanism of action, and use in the treatment of respiratory tract diseases. Am J Ther, 2002, 9(4): 317-328.
- Sodium salicylate
Catalog No.:BCC4846
CAS No.:54-21-7
- 5-Hydroxyindole-3-Acetic Acid
Catalog No.:BCC8285
CAS No.:54-16-0
- Tryptophan
Catalog No.:BCN2615
CAS No.:54-12-6
- L-Nicotine
Catalog No.:BCN6269
CAS No.:54-11-5
- Cefaclor
Catalog No.:BCC2527
CAS No.:53994-73-3
- Z-Phg-OH
Catalog No.:BCC2795
CAS No.:53990-33-3
- Luteolin 7,3'-di-O-glucuronide
Catalog No.:BCN5396
CAS No.:53965-08-5
- Ginsenoside F1
Catalog No.:BCN1244
CAS No.:53963-43-2
- Glycyrrhizic acid ammonium salt
Catalog No.:BCN5943
CAS No.:53956-04-0
- Aristolactam BIII
Catalog No.:BCN5718
CAS No.:53948-10-0
- Aristolactam BII
Catalog No.:BCN5717
CAS No.:53948-09-7
- Aristolactam AII
Catalog No.:BCN3924
CAS No.:53948-07-5
- Metyrapone
Catalog No.:BCC7632
CAS No.:54-36-4
- Idoxuridine
Catalog No.:BCC4666
CAS No.:54-42-2
- Pilocarpine HCl
Catalog No.:BCC4702
CAS No.:54-71-7
- Cinanserin hydrochloride
Catalog No.:BCC6653
CAS No.:54-84-2
- Isoniazid
Catalog No.:BCC9003
CAS No.:54-85-3
- Pentylenetetrazole
Catalog No.:BCC7453
CAS No.:54-95-5
- Amifampridine
Catalog No.:BCC5185
CAS No.:54-96-6
- Albendazole Oxide
Catalog No.:BCC4757
CAS No.:54029-12-8
- Etonogestrel
Catalog No.:BCC5230
CAS No.:54048-10-1
- Tofacitinib (CP-690550) Citrate
Catalog No.:BCC2189
CAS No.:540737-29-9
- Palosuran
Catalog No.:BCC4311
CAS No.:540769-28-6
- Isoastilbin
Catalog No.:BCN5719
CAS No.:54081-48-0
Peritoneal Dialysis vs Furosemide for Prevention of Fluid Overload in Infants After Cardiac Surgery: A Randomized Clinical Trial.[Pubmed:28241247]
JAMA Pediatr. 2017 Apr 1;171(4):357-364.
Importance: Fluid overload after congenital heart surgery is frequent and a major cause of morbidity and mortality among infants. Many programs have adopted the use of peritoneal dialysis (PD) for fluid management; however, its benefits compared with those of traditional diuretic administration are unknown. Objective: To determine whether infants randomized to PD vs Furosemide for the treatment of oliguria have a higher incidence of negative fluid balance on postoperative day 1, as well as avoidance of 10% fluid overload; shorter duration of mechanical ventilation, intensive care unit stay, and inotrope use; and fewer electrolyte abnormalities. Design, Setting, and Participants: This single-center, unblinded, randomized clinical trial compared methods of fluid removal after cardiac surgery from October 1, 2011, through March 13, 2015, in a large tertiary pediatric hospital in Ohio. The parents or guardians of all eligible infants (aged <6 months) undergoing cardiac surgery with catheter placement for PD were approached for inclusion. No patients were withdrawn for adverse effects. Recruitment was powered for the primary outcome, and analysis was based on intention to treat. Patients randomized to PD were hypothesized to have superior outcomes. Interventions: Infants received intravenous Furosemide (1 mg/kg every 6 hours) or a standardized PD regimen. Main Outcomes and Measures: The primary end point was incidence of negative fluid balance on postoperative day 1. Secondary end points included incidence of fluid overload, duration of mechanical ventilation and intensive care unit stay, electrolyte abnormalities and repletion doses, duration of inotropic administration, and mortality. Results: Seventy-three patients (47 boys [64%] and 26 girls [35%]; median age, 8 [interquartile range (IQR), 6-14] days) received treatment and completed the trial. No difference was found between the PD and Furosemide groups in the incidence of negative fluid balance on the first postoperative day. The Furosemide group was 3 times more likely to have 10% fluid overload (odds ratio [OR], 3.0; 95% CI, 1.3-6.9), was more likely to have prolonged ventilator use (OR, 3.1; 95% CI, 1.2-8.2), and had a longer duration of inotrope use (median, 5.5 [IQR, 4-8] vs 4.0 [IQR, 3-6] days) and higher electrolyte abnormality scores (median, 6 [IQR, 4-7] vs 3 [IQR, 2-5]) compared with the PD group. No statistically significant differences in mortality (3 patients [9.4%] in the Furosemide group vs 1 patient [3.1%] in the PD group) or length of cardiac intensive care unit (median, 7 [IQR, 6-12] vs 9 [IQR, 5-15] days) or hospital (15 [IQR, 10-28] vs 14 [IQR, 9-22] days) stay were observed. No serious complications were observed. Dialysis was discontinued early in 9 of 41 patients in the PD group for pleural-peritoneal communication. Conclusions and Relevance: Use of PD is safe and allows for superior fluid management with improved clinical outcomes compared with diuretic administration. Use of PD should be strongly considered among infants at high risk for postoperative acute kidney injury and fluid overload. Trial Registration: clinicaltrials.gov Identifer: NCT01709227.
Bolus Injection Versus Infusion of Furosemide in Kidney Transplantation: A Randomized Clinical Trial.[Pubmed:28299764]
Urol J. 2017 Mar 16;14(2):3013-3017.
PURPOSE: Furosemide is commonly administered to increase the urinary output in patients with transplanted kidneys. This study compared the two administration routes of Furosemide (bolus versus infusion) in kidney transplanted patients. MATERIALS AND METHODS: Fifty patients who had undergone kidney transplantation in 2015 in a hospital in Tabriz, Iran, were included in this clinical trial. They were divided into two groups: bolus (120 mg stat) and infusion (4 mg/minute) groups. The primary outcome was urine onset time. Secondary outcomes were urine output volume, vital signs (blood pressure, heart rate), and electrolyte level (creatinine, blood urea nitrogen, sodium and potassium). After arterial and venous anastomoses, arterial clamp removal time and diuresis onset were recorded. Finally, theurinary output volumes of both groups were measured with regular urine bags for an hour after anastomosis. Then it was repeated each three hours for 24 hours, and eventually two and three days thereafter. Finally, all data were statistically analyzed. RESULTS: Around 72% of the patients were men (mean age of 37.15 ± 14.67 years). Urine output was higher in bolus group but it was not statistically significant. Diuresis duration was measured after arterial declamping and its averages were 5.41 ± 3.7 minutes and 9.36 ± 7.65 minutes in bolus and infusion groups, respectively (P = .040). Furosemide bolus injection and infusion had no significant effect on creatinine, blood urea nitrogen, sodium and potassium. CONCLUSION: Furosemide bolus injection can reduce diuresis onset time compared to Furosemide infusion.
Population pharmacokinetic modeling of furosemide in patients with hypertension and fluid overload conditions.[Pubmed:28340405]
Pharmacol Rep. 2017 Jun;69(3):492-496.
BACKGROUND: Furosemide is a loop diuretic drug frequently indicated in hypertension and fluid overload conditions such as congestive heart failure and hepatic cirrhosis. OBJECTIVE: The purpose of the study was to establish a population pharmacokinetic model for Furosemide in Indian hypertensive and fluid overload patients, and to evaluate effects of covariates on the volume of distribution (V/F) and oral clearance (CL/F) of Furosemide. METHODS: A total of 188 Furosemide plasma sample concentrations from 63 patients with hypertension or fluid overload conditions were collected in this study. The population pharmacokinetic model for Furosemide was built using Phoenix NLME 1.3 software. The covariates included age, sex, body surface area, bodyweight, height and creatinine clearance (CRCL). RESULTS: The pharmacokinetic data of Furosemide was adequately explained by a two-compartment linear pharmacokinetic model with first-order absorption and an absorption lag-time. The mean values of CL/F and Vd/F of Furosemide in the patients were 15.054Lh(-1) and 4.419L, respectively. Analysis of covariates showed that CRCL was significantly influencing the clearance of Furosemide. CONCLUSION: The final population pharmacokinetic model was demonstrated to be appropriate and effective and it can be used to assess the pharmacokinetic parameters of Furosemide in Indian patients with hypertension and fluid overload conditions.
A retrospective evaluation of furosemide and mannitol for prevention of cisplatin-induced nephrotoxicity.[Pubmed:28276070]
J Clin Pharm Ther. 2017 Jun;42(3):286-291.
WHAT IS KNOWN AND OBJECTIVE: Nephrotoxicity is a recognized side effect of cisplatin chemotherapy. However, the optimal strategy for preventing cisplatin-induced nephrotoxicity, if any, remains unclear. The primary objective for this study was to determine whether mannitol or Furosemide provides better nephroprotection when administered with hydration prior to weekly, low-dose cisplatin concurrently with whole pelvic radiotherapy. METHODS: Clinical data were abstracted from all women who underwent chemoradiation for FIGO IB2-IVA cervical cancer at a regional safety net health system between January 2009 and December 2014. Creatinine clearance was estimated using the IDMS-traceable MDRD Study Equation. Descriptive statistics were used to summarize patient demographics. Cox proportional hazard models were used to identify factors associated with hypomagnesemia and survival. RESULTS AND DISCUSSION: A total of 133 women received 656 weekly doses of single-agent cisplatin (40 mg/m(2) ) concomitant with whole pelvic radiation. Furosemide (20 mg) was administered intravenously prior to 341 cisplatin doses, whereas mannitol (24 g) was administered prior to 315 doses. Significant magnesium wasting was observed after the second weekly cisplatin infusion regardless of whether Furosemide or mannitol was utilized. Repetitive low-dose cisplatin infusion had no impact on measured levels of serum creatinine or estimated glomerular filtration rate. Prior history of hypertension, diabetes mellitus, hepatitis C infection and acute gastrointestinal toxicity were each associated with early onset of hypomagnesemia. WHAT IS NEW AND CONCLUSIONS: Repetitive administration of low-dose cisplatin concurrent with whole pelvic radiation is associated with magnesium wasting. However, choice of diuretic with pretreatment hydration had no significant impact on the severity of this adverse effect.
Anticonvulsant actions of furosemide in vitro.[Pubmed:10391452]
Neuroscience. 1999;91(4):1471-81.
Anticonvulsant properties of Furosemide have been suggested to reduce neuronal synchronization via its inhibitory effect on the Na+/K+/2Cl- co-transport system. We have studied effects of Furosemide on spontaneous epileptiform activity and analysed effects of Furosemide on amplitudes of stimulus-induced population-spikes, on stimulus-induced K+ changes, on extracellular pH changes at rest and during stimulation, and on changes in the extracellular space-volume. We used three different in vitro models of epilepsy in the combined hippocampal-entorhinal cortex slice preparation. Furosemide reversibly suppressed low Ca2+-induced epileptiform activity in hippocampus proper and blocked or significantly reduced different types of epileptiform discharges in the low Mg2+ model and the 4-aminopyridine model. Amplitudes of evoked field potentials underwent an initial slight increase followed by a significant reduction after prolonged treatment with Furosemide. Stimulus-induced increases in extracellular potassium were also significantly reduced. Furosemide caused an alkaline shift at rest. Stimulus-induced pH transients changed from a biphasic alkalotic-acidotic sequence to a monophasic alkalotic shift. Stimulation-induced shrinkage of extracellular space-volume was reduced by Furosemide, whereas no effect on baseline extracellular space-volume was seen. We conclude, that Furosemide possesses strong anticonvulsive effects in various in vitro models of epilepsy. The anticonvulsive properties of Furosemide cannot be explained by its effects on extracellular pH changes but appear in part to be mediated via a reduced excitability with consequent reduction of activity-induced potassium rises. Finally, partial inhibition of activity-induced extracellular space shrinkage may contribute to its anticonvulsant properties.
Residues in transmembrane domains I and II determine gamma-aminobutyric acid type AA receptor subtype-selective antagonism by furosemide.[Pubmed:10347239]
Mol Pharmacol. 1999 Jun;55(6):993-9.
GABAA receptors in cerebellar granule cells are unique in expressing a subtype containing the alpha6 subunit. This receptor subtype has high affinity for GABA and produces a degree of tonic inhibition on cerebellar granule cells, modulating the firing of these cells via spillover of GABA from GABAergic synapses. This receptor subtype also has selective affinity for the diuretic Furosemide over receptors containing other alpha-subunits. Furosemide exhibits approximately 100-fold selectivity for alpha6-containing receptors over alpha1-containing receptors. By making alpha1/alpha6 chimeras we have identified a transmembrane region (209-279) responsible for the high Furosemide sensitivity of alpha6beta3gamma2s receptors. Within the alpha1 transmembrane region, a single amino acid was identified that when mutated from threonine to isoleucine, increased Furosemide sensitivity by 20-fold. We demonstrate the beta-subunit selectivity of Furosemide to be due to asparagine 265 in the beta2 and beta3 transmembrane-domain II similar to that observed with potentiation by the anticonvulsant loreclezole. We also show that Ile in transmembrane-domain I accounts for the increased GABA sensitivity observed at alpha6beta3gamma2s compared with alpha1beta3gamma2s receptors, but did not affect direct activation by pentobarbital or potentiation by the benzodiazepine flunitrazepam. Location of these residues within transmembrane domains leads to speculation that they may be involved in the channel-gating mechanism conferring increased receptor activation by GABA, in addition to conferring Furosemide sensitivity.


