Atazanavir sulfate (BMS-232632-05)Protease inhibitor CAS# 229975-97-7 |
- Saquinavir mesylate
Catalog No.:BCC1922
CAS No.:149845-06-7
- Amprenavir (agenerase)
Catalog No.:BCC3619
CAS No.:161814-49-9
- Tipranavir
Catalog No.:BCC2002
CAS No.:174484-41-4
- Lopinavir
Catalog No.:BCC3621
CAS No.:192725-17-0
- Atazanavir
Catalog No.:BCC3622
CAS No.:198904-31-3
- Narlaprevir
Catalog No.:BCC1785
CAS No.:865466-24-6
Quality Control & MSDS
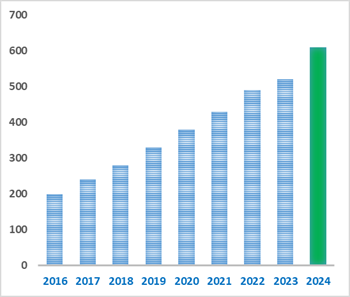
Number of papers citing our products
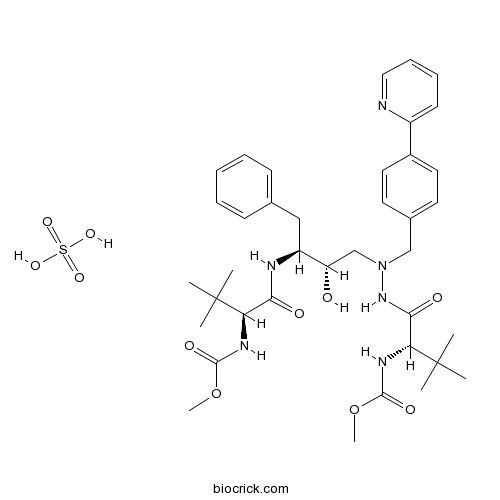
Chemical structure
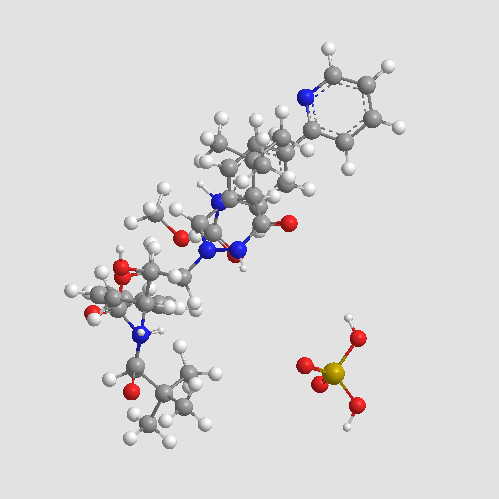
3D structure
| Cas No. | 229975-97-7 | SDF | Download SDF |
| PubChem ID | 158550 | Appearance | Powder |
| Formula | C38H54N6O11S | M.Wt | 802.9 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Synonyms | BMS-232632 sulfate | ||
| Solubility | Soluble to 104 mg/mL (129.52 mM) in DMSO | ||
| Chemical Name | methyl N-[(2S)-1-[2-[(2S,3S)-2-hydroxy-3-[[(2S)-2-(methoxycarbonylamino)-3,3-dimethylbutanoyl]amino]-4-phenylbutyl]-2-[(4-pyridin-2-ylphenyl)methyl]hydrazinyl]-3,3-dimethyl-1-oxobutan-2-yl]carbamate;sulfuric acid | ||
| SMILES | CC(C)(C)C(C(=O)NC(CC1=CC=CC=C1)C(CN(CC2=CC=C(C=C2)C3=CC=CC=N3)NC(=O)C(C(C)(C)C)NC(=O)OC)O)NC(=O)OC.OS(=O)(=O)O | ||
| Standard InChIKey | DQSGVVGOPRWTKI-QVFAWCHISA-N | ||
| Standard InChI | InChI=1S/C38H52N6O7.H2O4S/c1-37(2,3)31(41-35(48)50-7)33(46)40-29(22-25-14-10-9-11-15-25)30(45)24-44(43-34(47)32(38(4,5)6)42-36(49)51-8)23-26-17-19-27(20-18-26)28-16-12-13-21-39-28;1-5(2,3)4/h9-21,29-32,45H,22-24H2,1-8H3,(H,40,46)(H,41,48)(H,42,49)(H,43,47);(H2,1,2,3,4)/t29-,30-,31+,32+;/m0./s1 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Atazanavir sulfate is a sulfate salt form of atazanavir that is an highly potent HIV-1 protease inhibitor.
Target: HIV-1 protease inhibitor
Atazanavir sulfate is a sulfate salt form of atazanavir that is an highly potent HIV-1 protease inhibitor. It has a pharmacokinetic profile that supports once-daily dosing and has demonstrated a unique resistance profile and superior virologic potency compared with other antiretrovirals in vitro. In subjects with HIV, atazanavir (400 mg once daily) produced rapid and sustained improvements in viral load and CD4 counts in both antiretroviral-naive as well as previously treated patients when used in combination with dual nucleoside reverse transcriptase inhibitor (NRTI) treatment [1].
After intravenous (iv), oral (po) and intraportal (ip) administration of ATV at a dosage of 7 mg/kg, AUCs in HL rats were 12.41, 5.24 and 8.89 microg/mLh, respectively, and were significantly higher than those in control rats (4.09, 1.70 and 3.38 microg/mLh). Despite the decrease of distribution volume (Vd(ss)), the terminal half-life (t(1/2)) in HL tended to be shorter than in control, and hepatic distribution of ATV in HL rats was 4.8-fold increases. These results suggested that the uptake of ATV into liver might counteract the decrease of Vd(ss). On the other hand, there was no significant difference in bioavailability, and the lymphatic transport to AUC showed no statistical change. In conclusion, although the protein binding rate and AUC were significantly increased, the pharmacokinetics of ATV might be tolerated in HL [2].
Clinical indications: HIV-1 infection
Toxicity: torsades de pointes References: | |||||

Atazanavir sulfate (BMS-232632-05) Dilution Calculator

Atazanavir sulfate (BMS-232632-05) Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 1.2455 mL | 6.2274 mL | 12.4549 mL | 24.9097 mL | 31.1371 mL |
| 5 mM | 0.2491 mL | 1.2455 mL | 2.491 mL | 4.9819 mL | 6.2274 mL |
| 10 mM | 0.1245 mL | 0.6227 mL | 1.2455 mL | 2.491 mL | 3.1137 mL |
| 50 mM | 0.0249 mL | 0.1245 mL | 0.2491 mL | 0.4982 mL | 0.6227 mL |
| 100 mM | 0.0125 mL | 0.0623 mL | 0.1245 mL | 0.2491 mL | 0.3114 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||
Calcutta University

University of Minnesota

University of Maryland School of Medicine
University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University
DRURY University
Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University
The University of Tokyo

Korea University
Atazanavir sulfate (BMS-232632-05) is the sulfate salt form of atazanavir, a potent protease inhibitor (IP) for the treatment of human immunodeficiency virus 1 (HIV-1) infection, which prevents the formation of mature HIV virions through the selective inhibition of the virus-specific processing of viral gag and gag-pol polyproteins in infected cells. Although it shows strong anti-HIV-1 activity with MIC50 ranging from 2 to 5 nM, atazanavir has lower antiviral activity against HIV-2 isolates. Atazanavir, which is metabolized by the hepatic cytochrome P450 (CYP) system resulting in two main inactive metabolites, is also an inhibitor of CYP3A4 isoenzyme and P-glycoprotein ATP-dependent efflux pump.
Reference
Robin Wood. Atazanavir: its role in HIV treatment. Expert Rev Snti Infect Ther 2008; 6(6): 785-796
- AGN 194310
Catalog No.:BCC5416
CAS No.:229961-45-9
- GW9662
Catalog No.:BCC2260
CAS No.:22978-25-2
- Abn-CBD
Catalog No.:BCC7011
CAS No.:22972-55-0
- Desmethoxycentaureidin
Catalog No.:BCN5077
CAS No.:22934-99-2
- Neferine
Catalog No.:BCN6338
CAS No.:2292-16-2
- Ginkgolic acid C15:1
Catalog No.:BCN2307
CAS No.:22910-60-7
- R 892
Catalog No.:BCC5992
CAS No.:229030-05-1
- TAK-779
Catalog No.:BCC4137
CAS No.:229005-80-5
- 4-Amino-3,5-dichloropyridine
Catalog No.:BCC8679
CAS No.:22889-78-7
- Silymarin
Catalog No.:BCN6299
CAS No.:22888-70-6
- Famprofazone
Catalog No.:BCC3779
CAS No.:22881-35-2
- 6-Acetonyldihydrochelerythrine
Catalog No.:BCN5076
CAS No.:22864-92-2
- MPTP hydrochloride
Catalog No.:BCC1778
CAS No.:23007-85-4
- Neoglycyrol
Catalog No.:BCN2907
CAS No.:23013-84-5
- Physalin A
Catalog No.:BCN7920
CAS No.:23027-91-0
- Apelin-36 (rat, mouse)
Catalog No.:BCC5911
CAS No.:230299-95-3
- Terbutaline Sulfate
Catalog No.:BCC4320
CAS No.:23031-32-5
- Z-β-Ala-OH
Catalog No.:BCC3058
CAS No.:2304-94-1
- Z-Asn-OH
Catalog No.:BCC2794
CAS No.:2304-96-3
- Z-Arg(NO2)-OH
Catalog No.:BCC3063
CAS No.:2304-98-5
- Ajugasterone C
Catalog No.:BCN2757
CAS No.:23044-80-6
- Lofepramine
Catalog No.:BCC7402
CAS No.:23047-25-8
- Dihydroconiferyl alcohol
Catalog No.:BCN7047
CAS No.:2305-13-7
- L-AP4
Catalog No.:BCC6550
CAS No.:23052-81-5
Drug resistance testing through remote genotyping and predicted treatment options in human immunodeficiency virus type 1 infected Tanzanian subjects failing first or second line antiretroviral therapy.[Pubmed:28582463]
PLoS One. 2017 Jun 5;12(6):e0178942.
INTRODUCTION: Antiretroviral therapy (ART) has been successfully introduced in low-middle income countries. However an increasing rate of ART failure with resistant virus is reported. We therefore described the pattern of drug resistance mutations at antiretroviral treatment (ART) failure in a real-life Tanzanian setting using the remote genotyping procedure and thereafter predicted future treatment options using rule-based algorithm and the EuResist bioinformatics predictive engine. According to national guidelines, the default first-line regimen is tenofovir + lamivudine + efavirenz, but variations including nevirapine, stavudine or emtricitabine can be considered. If failure on first-line ART occurs, a combination of two nucleoside reverse transcriptase inhibitors (NRTIs) and boosted lopinavir or atazanavir is recommended. MATERIALS AND METHODS: Plasma was obtained from subjects with first (n = 174) or second-line (n = 99) treatment failure, as defined by clinical or immunological criteria, as well as from a control group of ART naive subjects (n = 17) in Dar es Salaam, Tanzania. Amplification of the pol region was performed locally and the amplified DNA fragment was sent to Sweden for sequencing (split genotyping procedure). The therapeutic options after failure were assessed by the genotypic sensitivity score and the EuResist predictive engine. Viral load was quantified in a subset of subjects with second-line failure (n = 52). RESULTS: The HIV-1 pol region was successfully amplified from 55/174 (32%) and 28/99 (28%) subjects with first- or second-line failure, respectively, and 14/17 (82%) ART-naive individuals. HIV-1 pol sequence was obtained in 82 of these 97 cases (84.5%). Undetectable or very low (<2.6 log10 copies/10-3 L) viral load explained 19 out of 25 (76%) amplification failures in subjects at second-line ART failure. At first and second line failure, extensive accumulation of NRTI (88% and 73%, respectively) and NNRTI (93% and 73%, respectively) DRMs but a limited number of PI DRMs (11% at second line failure) was observed. First line failure subjects displayed a high degree of cross-resistance to second-generation NNRTIs etravirine (ETR; 51% intermediate and 9% resistant) and rilpivirine (RPV; 12% intermediate and 58% resistant), and to abacavir (ABC; 49% resistant) which is reserved for second line therapy in Tanzania. The predicted probability of success with the best salvage regimen at second-line failure decreased from 93.9% to 78.7% when restricting access to the NRTIs, NNRTIs and PIs currently available in Tanzania compared to when including all approved drugs. DISCUSSION: The split genotyping procedure is potential tool to analyse drug resistance in Tanzania but the sensitivity should be evaluated further. The lack of viral load monitoring likely results in a high false positive rate of treatment failures, unnecessary therapy switches and massive accumulation of NRTI and NNRTI mutations. The introduction of regular virological monitoring should be prioritized and integrated with drug resistance studies in resource limited settings.
Atazanavir-Associated Crystalline Nephropathy.[Pubmed:28579422]
Am J Kidney Dis. 2017 Oct;70(4):576-580.
Crystalline nephropathy can occur following treatment with multiple therapeutic agents. We describe a human immunodeficiency virus (HIV)-infected patient treated for 2 years with combination antiretroviral therapy including atazanavir (ATV). Kidney biopsy revealed a crystalline nephropathy associated with diffuse chronic and granulomatous interstitial inflammation. Following the biopsy, treatment with ATV was discontinued and kidney function returned to pretreatment baseline levels. ATV, which has a well-established association with nephrolithiasis, is a rare but important cause of crystalline nephropathy. Recognition of this association and prompt withdrawal of the offending agent are critical to optimize outcomes.
A cross-sectional study to evaluate second line virological failure and elevated bilirubin as a surrogate for adherence to atazanavir/ritonavir in two urban HIV clinics in Lilongwe, Malawi.[Pubmed:28673254]
BMC Infect Dis. 2017 Jul 3;17(1):461.
BACKGROUND: Malawi's national antiretroviral therapy program provides atazanavir/ritonavir-based second line regimens which cause concentration-dependent rise in indirect bilirubin. We sought to determine if elevated bilirubin, as a surrogate of atazanavir/ritonavir adherence, can aid in the evaluation of second line virological failure in Malawi. METHODS: We conducted a cross-sectional study of HIV-infected patients >/=15 years who were on boosted protease inhibitor-based second line antiretroviral therapy for at least 6 months in two urban HIV clinics in Lilongwe, Malawi. Antiretroviral therapy history and adherence data were extracted from the electronic medical records and blood was drawn for viral load, complete blood count, total bilirubin, and CD4 cell count at a clinic visit. Factors associated with virological failure were assessed using multivariate logistic regression model. RESULTS: Out of 376 patients on second line antiretroviral therapy evaluated, 372 (98.9%) were on atazanavir/ritonavir-based therapy and 142 (37.8%) were male. Mean age was 40.9 years (SD +/- 10.1), mean duration on second line antiretroviral therapy was 41.9 months (SD +/- 27.6) and 256 patients (68.1%) had elevated bilirubin >1.3 mg/dL. Overall, 35 (9.3%) patients had viral load >1000 copies/ml (virological failure). Among the virologically failing vs. non-failing patients, bilirubin was elevated in 34.3% vs. 72.0% respectively (p < 0.001), although adherence by pill count was similar (62.9% vs. 60.7%, p = 0.804). The odds of virological failure were higher for adults aged 25-40 years (adjusted odds ratio (aOR) 2.5, p = 0.048), those with CD4 cell count <100 (aOR 17.5, p < 0.001), and those with normal bilirubin levels (aOR 5.4, p < 0.001); but were lower for the overweight/obese patients (aOR 0.3, p = 0.026). Poor pill count adherence (aOR 0.7, p = 0.4) and male gender (aOR 1.2, p = 0.698) were not associated with second line virological failure. CONCLUSIONS: Among patients receiving atazanavir/ritonavir-based second line antiretroviral therapy, bilirubin levels better predicted virological failure than pill count adherence. Therefore, strategic use of bilirubin and viral load testing to target adherence counseling and support may be cost-effective in monitoring second line antiretroviral therapy adherence and virological failure. Drug resistance testing targeted for patients with virological failure despite elevated bilirubin levels would facilitate timely switch to third line antiretroviral regimens whenever available.
Atazanavir sulfate + cobicistat for the treatment of HIV infection.[Pubmed:28443391]
Expert Rev Anti Infect Ther. 2017 Jun;15(6):569-576.
INTRODUCTION: During last two decades several drugs were developed to offer long-term benefits in terms of virologic efficacy, favourable tolerability and toxicity profiles in treatment of HIV infection. Pharmacokinetics boosting of protease inhibitor allows a higher genetic barrier, as few or no drug-resistant mutations are detected in patients with virologic failure. Areas covered: Atazanavir sulfate + cobicistat (ATV/c) was recently approved for the treatment of HIV-1 infection. Bioequivalence between cobicistat (COBI) and ritonavir (RTV) as a pharmacoenhancer of ATV was established. Additionally, randomized clinical trials demonstrated that ATV/c and ATV/ritonavir had comparable efficacy and safety profiles. Low rates of virologic failure and no ATV resistance mutations were observed in these clinical trials. Therefore, COBI shows increased advantages over RTV, such as no activity against HIV, fewer drug-drug interactions and better solubility, which promotes coformulation strategies with less pill burden, better tolerability, and, potentially, higher life-long treatment adherence. Expert commentary: ATV/c regimen supports its useas an effective treatment option for HIV-1 infected patients with increased cardiovascular disease and chronic kidney disease risk associated with aging. In addition, ATV/c is a new opportunity to expand the strategy of switch to a dual therapy to lower the risk of long-term toxicities as well as the advantage of its cost-benefit.
Second- and Third-line Antiretroviral Therapy for Children and Adolescents: A Scoping Review.[Pubmed:28403052]
Pediatr Infect Dis J. 2017 May;36(5):492-499.
BACKGROUND: The World Health Organization identified a need for evidence to inform revision of second- and third-line antiretroviral therapy (ART) options in children failing ART. We performed an in-depth scoping review of all available literature on second-line and subsequent ART regimens in children younger than 18 years. METHODS: We comprehensively searched, without language or date limitations, the Cochrane Central Register of Controlled Trials, MEDLINE, EMBASE, the World Health Organization's International Clinical Trials Registry Platform and ClinicalTrials.gov. RESULTS: The search retrieved 1982 records. Eighteen studies provided efficacy data: 1 randomized controlled trial, 7 phase II trials, 5 prospective and 5 retrospective cohorts. Five studies evaluated regimens in children failing first-line ART, 4 in children with multidrug resistance and 9 in children with variable treatment experience. Only 10/18 studies reported week 48 or month 12 outcomes. The overall proportion of children with virologic suppression defined by study at week 48 was 61.8%. Although the randomized controlled trial had low risk of bias, outcomes were similar between groups because of highly active optimized background regimens. All phase II and prospective studies were judged to have moderate to high risk of bias. No study compared currently recommended lopinavir-based second-line regimens for nonnucleoside reverse transcriptase inhibitor failures to other non-nonnucleoside reverse transcriptase inhibitor regimens head-to-head. CONCLUSIONS: We found no evidence comparing current World Health Organization-recommended second- and third-line ART regimens with regimens including drugs of interest: raltegravir, darunavir, etravirine and atazanavir. Randomized controlled trials or prospective cohort studies with comparator arms, and bridging studies, ideally conducted in resource-limited settings, are required to guide future recommendations.


